St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
The ability to manipulate genetic material to introduce a specific change or edit has already proven transformative in biomedical science — with even more groundbreaking possibilities on the horizon.

The liquid handler in the Center for Advanced Genome Engineering (CAGE) facilitates high throughput experimentation.
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) technology has emerged as a game-changer in research. It is a powerful tool for studying the genetic underpinnings of various diseases and consequently paves the way for developing novel therapeutic interventions.
The technology’s impact was exemplified in 2020, when the Nobel Prize in Chemistry was awarded to Emmanuelle Charpentier, PhD, a former St. Jude postdoctoral fellow, and Jennifer Doudna, PhD, for their roles in its development. CRISPR has made it possible to edit genes in living organisms with unprecedented precision and efficiency, significantly accelerating the pace of scientific discovery.
The system has two main components: a guide RNA and a DNA-cutting enzyme called Cas protein. The guide RNA mirrors the gene’s DNA sequence to be edited (the target). Working together, the guide RNA and Cas protein locate the target gene. Once the guide RNA aligns with the target gene’s DNA, the Cas protein precisely cuts the DNA at the target site.
At St. Jude, CRISPR has propelled cutting-edge research in cancer, immunity, and the fundamental mechanisms of transcription and gene regulation. Transcription is an essential biological process in which DNA is copied into RNA. This process is the first required step a cell takes to access the code housed in DNA and ultimately translate that code into the amino acid or polypeptide building blocks that become active proteins. Dysregulated transcription plays a role in many types of pediatric cancer.

Instead of testing each of the hundreds of thousands of unique drug–drug combinations, we’re using CRISPR gene editing to knock out genes that we already know to be druggable, then giving those neuroblastoma cells a known chemotherapeutic to look for synergistic effects.
Department of Computational Biology.
The interaction between departments and Shared Resources has been instrumental in driving these advancements. In the Center for Advanced Genome Engineering (CAGE), a shared resource led by Shondra Pruett-Miller, PhD, a team of CRISPR experts provides their guidance and technological capabilities to the entire research enterprise. Combining this powerful technology with the biological questions posed in St. Jude research labs is advancing our understanding of human health and disease.
CRISPR reveals new strategies to treat cancer
Cancer cells change and adapt, which makes the disease insidious and challenging to treat. Neuroblastoma, a childhood solid tumor that affects multiple tissues, is prone to relapse and resistance; 40% to 50% of affected children experience a return of their cancer after treatment is completed. Single chemotherapy agents are often insufficient for treating cancer due to drug resistance. However, combination therapy, which uses multiple drugs with different mechanisms of action, decreases the likelihood of cancer cells developing resistance, thus maximizing treatment efficacy.
Employing CRISPR technology, St. Jude researchers developed a new roadmap for the use of combination chemotherapy in patients with high-risk neuroblastoma. With thousands of available drugs and compounds, screening for combinations to enhance the standard of care in a particular disease setting is challenging. In Nature Communications, St. Jude researchers reported using large-scale targeted CRISPR knockout screens to study various combinations of drugs in cancer cell lines.
“Instead of testing each of the hundreds of thousands of unique drug–drug combinations, we’re using CRISPR gene editing to knock out genes that we already know to be druggable, then giving those neuroblastoma cells a known chemotherapeutic to look for synergistic effects,” said Paul Geeleher, PhD, Department of Computational Biology.
The investigators found that blocking PRKDC expression in isolated neuroblastoma cells made them vulnerable to doxorubicin, a chemotherapy. They then demonstrated that using both doxorubicin and a PRKDC inhibitor in mouse models of neuroblastoma had a synergistic effect, which means that the combination of the two drugs controlled tumor growth more effectively than either drug alone.
“The goal, ultimately, is to find better treatments that are more targeted with less toxicity,” said Adam Durbin, MD, PhD, Department of Oncology. “Plus, we want to find effective treatments for children with relapsed disease so that kids can grow up without problems related to high-intensity neuroblastoma therapy.”

A scientist returns flasks of cell lines to an incubator in CAGE.
With so many potential drug combinations largely untapped, screening for novel multidrug approaches could be transformative for neuroblastoma and other difficult-to-treat cancers.
CRISPR–Cas9 screening has also been instrumental in creating disease models suitable for studying and developing potential therapeutic targets in humans. Although liver cancers are rare among children, hepatoblastoma is becoming more common. A steady rise in prevalence has been observed globally among children younger than 5 years, including a notable increase of over 4.3% annually in U.S. patients with high-risk hepatoblastoma, which is commonly treated with chemotherapy. Thus, novel treatment options are needed. It is crucial to establish a reliable and easily accessible research model to advance cancer treatment strategies.
In Nature Communications, St. Jude investigators used a newly developed mouse model to identify the genetic mutations underlying hepatoblastoma driven by the MYC family of proteins. The model enabled the team to perform a genome-wide CRISPR–Cas9 screen to identify the genes required for tumor cell survival. They identified over 1,500 genes as potential targets, with 100 preexisting inhibitors of these genes available.
“This means we can find many targets to test. Any researchers with a shared interest can use our detailed screening information to verify their hypotheses and develop new therapies,” said Jun Yang, PhD, Department of Surgery.
The CRISPR screen yielded potential targets that may enhance treatment efficacy when targeted in combination with conventional chemotherapy, such as doxorubicin, including PRKDC inhibition and increased DNA damage within tumor cells. This study sheds light on improving treatment outcomes for patients with hepatoblastoma and offers promising avenues for future therapies.
CRISPR and the immune system
In addition to helping researchers determine which therapies are most likely to succeed against different cancer types, CRISPR technology is a powerful tool that helps scientists better understand the immune response — the body’s natural defense mechanism that can react to cancer cells and promote their killing. Hongbo Chi, PhD, Department of Immunology, conducts research on the immune system by exploring how T cells function to kill cancer cells.

Shilpa Narina, lead researcher in CAGE, uses state-of-the-art liquid handling robot to conduct high-throughput CRISPR screens.
In Nature, Chi and his team reported using single-cell CRISPR screens to map gene regulatory networks involved in anti-tumor immunity. This approach enabled the researchers to conduct a comprehensive examination of transcription factors, which mediate gene regulation, linked to the T-cell’s anticancer response. They sought to understand mechanisms underlying T-cell exhaustion, which reduces the T-cell’s effectiveness against cancer cells.
The researchers also used this approach to study the gene regulatory networks involved in T-cell differentiation, a process that regulates T-cell function. They found that precisely perturbing the differentiation process could enhance anti-tumor efficacy. Specifically, they could increase the number of cancer-killing T cells by promoting differentiation to an intermediate T-cell state and blocking terminal differentiation.

“Such a causal transcriptional network provides new insights into lineage differentiation, a fundamental process in biology. The same approach may be more broadly applicable to increase our knowledge in many biological contexts beyond T cells and immunology. We showed this new technology, single-cell CRISPR screening in vivo, can drive novel biological discovery. I think we’re at the advent of something truly exciting.”
Department of Immunology
“We’ve provided new potential strategies to enhance immunotherapy,” said Peipei Zhou, PhD, a postdoctoral fellow in Chi’s lab. “We increased the amount of functionally competent cancer-killing T cells by differentiating them from upstream precursors or blocking their terminal differentiation.”
Hao Shi, PhD, a senior bioinformatics research scientist in the Department of Immunology, said, “The study generated a comprehensive T-cell differentiation map, which will be a valuable resource for future research, guiding scientists in enhancing T-cell–based immunotherapies.”
“Such a causal transcriptional network provides new insights into lineage differentiation, a fundamental process in biology,” Chi said. “The same approach may be more broadly applicable to increase our knowledge in many biological contexts beyond T cells and immunology. We showed this new technology, single-cell CRISPR screening in vivo, can drive novel biological discovery. I think we’re at the advent of something truly exciting.”
This comprehensive approach offers new strategies to improve T-cell–based immunotherapies that target cancer and other diseases and to guide future research. The study also underscores the potential of in vivo single-cell CRISPR screening in driving novel biological discoveries.
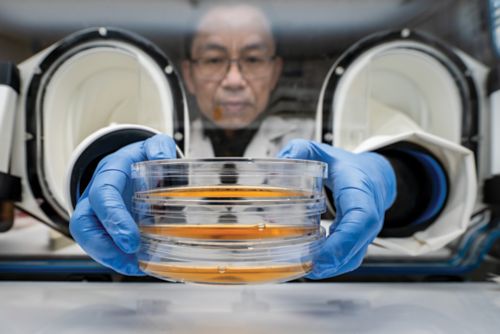
Jie Fang, PhD, scientist in CAGE, prepares samples for CRISPR screens.
CRISPR sheds light on cellular mechanisms
As Chi and his team use CRISPR to understand the factors important in regulating immune response, Chunliang Li, PhD, Department of Tumor Cell Biology, and colleagues are employing CRISPR technology to address key questions in the transcriptional regulation of cancer cells.
KMT2A-rearranged leukemia is a high-risk subtype of the disease that comprises about 10% of all acute leukemia cases and is found in over 80% of infant acute leukemias. The HOXA9 protein is a key dependency in these high-risk leukemias, but directly targeting HOXA9 is challenging. Published in Nature Communications, a report from Li’s group meticulously unraveled the transcriptional regulation network orchestrated by HOXA9.
The researchers used dropout CRISPR screens to focus on how HOXA9 binds to noncoding regulatory sequences of DNA and subsequently controls downstream genes crucial for cell survival. They found that HOXA9-associated regulatory programs influence leukemia cell dependency and provided new insights into regulation mechanisms.
“We confirmed two major known targets, FLT3 and CDK6,” said Li. “Both genes can be therapeutically targeted by drugs, which shows good outcomes in preclinical models with HOXA9 overexpression. Our results provided direct evidence to support the enhancer regulation of FLT3 and CDK6 through HOXA9.”
Li’s lab also uses CRISPR technology to identify novel treatment strategies for KMT2A-rearranged leukemia. Patients with KMT2A-rearranged leukemia have few treatment options. Bromo- and extra-terminal domain inhibitors (BETi) have shown promise but are prone to resistanc CRISPR.

Our expertise in combinatorial CRISPR screens allowed us to identify resistance mechanisms, but by also doing reverse screens, we identified the targetable options that will allow us to overcome resistance.
Department of Tumor Cell Biology
In a paper published in the Proceedings of the National Academy of Sciences USA, Li’s team used genome-wide CRISPR screens to investigate how leukemia cells with KMT2A rearrangements respond to BETi. They found that a lack of the protein SPOP is the main reason for resistance to BETi.
“Our expertise in combinatorial CRISPR screens allowed us to identify resistance mechanisms, but by also doing reverse screens, we identified the targetable options that will allow us to overcome resistance,” said Li.
Further CRISPR analysis suggested that inhibiting another protein called GSK3 could make the cancer cells sensitive to BETi again. Combining drugs that target both BET and GSK3 slowed the progression of leukemia and caused minimal toxicity in mice.
Digging deeper into the fundamental mechanisms of transcription and gene regulation, Li and his team used CRISPR and other cutting-edge technologies to better understand CTCF’s role in those processes. Although the biology of CTCF has been studied extensively, it was unclear how the different domains (parts) of CTCF function in relation to transcription regulation.

Microscopy equipment enables scientists to examine cell populations in vitro.
One of the most valuable ways to study a protein is to degrade, or remove, it from a model system and then study the functional changes that occur in its absence, providing insight into how the protein influences a cell. One system for degrading proteins is the auxin-inducible degron 1 (AID1) system. However, this system has limitations. Li’s work, published in Genome Biology, used the second-generation system, AID2, and a CRISPR single-guide RNA library screen to gain insight into the functional domains of CTCF.
The researchers found that depleting CTCF led to small changes, particularly in regions that play essential roles in controlling gene activity. The findings further show that the CTCF protein not only relies on binding to the DNA through the recognition of the CTCF DNA-binding motif but also relies on certain domains to bind to specific sequences flanking the motif. For a subset of genes, transcription is regulated only when CTCF binds to these specific sequences.
“When the CTCF protein is gone, we and others have observed that very few genes transcriptionally change,” Li said. “We know when we remove most of the CTCF protein in cells, the impact on transcription is minimal. So, the disconnect between the depletion of protein and transcription must follow a mechanism. We identified part of the mechanism.”
The CRISPR era is now
The innovative use of CRISPR technology at St. Jude is revolutionizing biomedical research. From identifying combination treatment approaches to learning how the immune system responds to cancer or gaining novel insights into fundamental mechanisms of gene regulation that can be exploited therapeutically — CRISPR is opening new options for treating disease. At St. Jude, CRISPR expertise is available to all researchers through the Center for Advanced Genome Engineering and has quickly become the backbone of discovery in many laboratories. The boundaries of CRISPR’s potential have not yet been realized. With expertise, technical capability, and laboratory resources at their disposal, St. Jude scientists are charting the future of disease treatment using CRISPR.