St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Following the breadcrumbs: Gain-of-function mutation leads researchers to new therapeutic target for pediatric AML
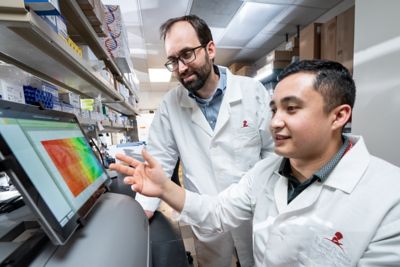
Pediatric acute myeloid leukemia (pAML) is distinct from adult AML. Jeffery Klco, MD, PhD (left), and Juan Barajas, PhD (right), explored genes uniquely linked to pAML and tracked a gain-of-function mutation in one protein with therapeutic potential
Often, in research, data will reflect simple majorities. Acute myeloid leukemia (AML) is a cancer tied to the process of hematopoiesis (blood cell development), and the average age of those who develop AML is about 65 years. Because of this, our understanding of the disease largely stems from our knowledge of its development in adults. However, only viewing AML as a disease of adults skews research — because children develop AML, too.
Despite representing a smaller percentage of overall AML, pediatric AML (pAML) accounts for 20% of pediatric leukemia and is associated with very poor patient outcomes, especially if relapse occurs. There is a large gap between our understanding of pAML and adult AML. The disproportionate impact of AML on older generations means that AML research often ignores or at least doesn’t consider the unique but smaller quantity of pAML cases. This affects patient outcomes as treatment for pAML could be improved by a better mechanistic understanding of the disease.
Jeffery Klco, MD, PhD, St. Jude Department of Pathology, and his team have been addressing these issues with an explicit goal propelling their research and collaborative efforts forward: understanding what makes pAML different from adult AML.
Digging into pediatric AML genetics
The genetic traits that make pAML cases so distinct were recently brought to light by Klco and his team and served as a call to action to give pAML the attention it deserves. Exploring the disease’s genetic landscape, Klco’s team categorized it into 23 molecular categories, including 12 new ones currently unrecognized by the present World Health Organization (WHO) classification system for AML.
“We recognized that many of the recurrent alterations we found in pAML aren’t even mentioned in the WHO classifications,” Klco said of the investigation, “even though some of these unrecognized subtypes have a significant impact on outcomes.”
One such subtype involves the gene UBTF (upstream binding transcription factor). UBTF encodes for a protein critical in ribosomal RNA transcription. In a subset of pAML, UBTF mutates by undergoing a type of DNA replication error called a tandem duplication. These genetic duplications involve exon 13 of UBTF and vary in size but lead to a functional yet mutated protein. This subtype was originally described in 2022 in Blood Cancer Discovery by Klco’s lab in collaboration with Xiaotu Ma, PhD, St. Jude Department of Computational Biology.
In early work examining UBTF and its role in pAML, Klco and his team noticed mechanistic breadcrumbs that ultimately helped them uncover the role of UBTF tandem duplications (UBTF-TD) in pAML.
“We recognized that there were features of these leukemias that we thought would give some indication as to the mechanism,” Klco explained. “In particular, how they expressed a certain subset of genes.”
Juan Barajas, PhD, a post-doctoral fellow along with other members of Dr. Klco’s lab, set out to follow the biological breadcrumbs and get to the bottom of UBTF-TD.
Understanding UBTF tandem duplication in pediatric AML
“For UBTF, the tandem duplication mutation is interesting because it results in a functional protein,” said Barajas, first author of a recent work published in Blood.
When a disease-linked protein doesn’t function, this “loss-of-function” mechanism can indicate why the disease occurs: A protein isn’t working. A functioning protein after tandem duplication indicated that instead of a loss-of-function causing disease, the researchers were possibly looking at a gain-of-function mechanism, where the mutated protein was doing something additional or different from the normal protein, and that function was contributing to the pAML.
Following the biological breadcrumbs led the researchers to the HOX genes. This family of genes is dysregulated in numerous cancers, including UBTF-TD pAML and other pAML subtypes. It seemed to Klco and his team that HOX genes also played a role in UBTF-linked pAML.
They tracked the mutated UBTF protein to the HOXA and HOXB gene clusters and got their answer.
“Juan set up some really elegant models to show that this mutant protein will directly bind to the HOXA and HOXB loci, or the gene location on the chromosome, whereas the wild type doesn’t,” said Klco, co-corresponding author on the paper.
Getting a clear picture of UBTF mechanism
Their studies further uncovered additional partners in crime. Along with the mutant UBTF interacting with HOX genes, the researchers found that two other proteins, KMT2A and Menin, can be found alongside mutated UBTF at these HOX loci. This finding was not particularly surprising to the researchers. KMT2A, a protein involved in hematopoiesis, and Menin, a protein linked to gene regulation, are often implicated in HOX-related leukemias.
The relationship between these two proteins and UBTF is a question Klco’s team aims to tackle.
While more is still to be revealed biologically, the findings are immediately exciting from a therapeutic point of view.
“The major challenges in treating relapsed AML include a lack of therapeutic targets and targeted therapy,” said Jeffrey Rubnitz, MD, PhD, St. Jude Department of Oncology, co-author on the paper. Drugs already exist that are designed to disrupt the Menin-KMT2A interaction, however.
“This work addresses the challenges in treatment by identifying UBTF-TD as a previously unrecognized target and demonstrating that UBTF-TD-positive leukemias are sensitive to treatment with Menin inhibitors,” expressed Rubnitz.
“Disrupting the Menin and KMT2A interactions, specifically, results in disruption of UBTF binding to the genome,” Barajas added. This disruption presents a potential route to treating patients with UBTF-TD pAML.
“This is a relatively new entity, however,” Barajas said. “So, there’s still a lot of work that needs to be done to fully understand what’s going on mechanistically.”
Expanding the scope of UBTF alterations in myeloid tumors
Klco and his team have also quickly built on their work with a follow-up publication in Haematologica outlining the clinicopathological features of pediatric myeloid tumors with UBTF alterations. In addition to expanding the cohort of pAML patients with UBTF tandem duplications, they also noted for the first time that similar duplications are also present in children and young adults with myelodysplastic syndrome (MDS). MDS is a condition wherein abnormal development of blood cells leads to atypical appearances (dysplasia). MDS can serve as a steppingstone to AML. Fittingly, patients with UBTF-mutated AML also have cellular dysplasia, which is overall rare in pAML.
By analyzing genomic data from the largest cohort of UBTF-TD–positive patients to date, the team observed a unique combination of accompanying mutations including the FLT3 and WT1 genes. These mutations led the cancer cells to exhibit stem cell-like features, which may bridge the gap between the observed transcriptional profiles of the disease and the dismal clinical outcomes exhibited in patients.
The detection of UBTF tandem duplications remains a challenge for many clinical labs. Since this is a newer entity that is enriched in children, many commercial labs that offer genetic testing do not test for UBTF mutations. Plus, the accurate detection of this alteration in sequencing data, which the Klco lab and collaborators have largely established, also remains problematic. Further complicating this situation is the recognition by the Klco lab that UBTF alterations can also be found outside of exon 13 in UBTF. In the recent Haematologica study, the group also described rare cases of pAML with a duplication involving exon 9, implying a potential shared mechanism and potential treatment options for those with exon 13 duplications.
“This collective work describes a new class of mutations that result in AML and MDS in children whose recognition can significantly impact how these children are clinically managed,” Klco said. “It’s well known that kids with these alterations have a dismal outcome. We look forward to helping the greater community to appropriately identify these mutations to maximize the benefits to patients.”






