St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Blocking the progression of pre-leukemic disorders
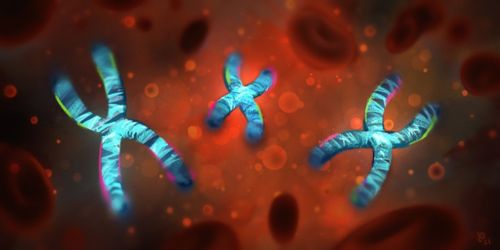
In his new lab at St. Jude John Crispino, PhD, is investigating the genetic underpinnings of pre-leukemic disorders, including how Down syndrome driven by a third copy of chromosome 21 predisposes children to leukemia.
As a student, John Crispino, PhD, wanted to apply a background in basic science to questions in medicine. He was drawn to studying hematopoiesis, the biological process that creates blood cells. This led to a robust career researching the biology of blood cells and the genetic changes that can lead these cells down a path to cancer.
Crispino’s work focuses on what causes leukemia to develop. This includes acute leukemia in children with Down syndrome due to an extra copy of chromosome 21, and pre-leukemic disorders like myelodysplastic syndrome (MDS) and myeloproliferative neoplasms (MPNs) that can become acute myeloid leukemia (AML). Crispino’s laboratory also works to develop novel, targeted therapies for children with blood disorders.
Since joining St. Jude in the summer of 2020, Crispino has published research that sheds light on these areas. One paper, in the Journal of Clinical Investigation, identified a drug target for B-cell leukemia, including leukemia in children with Down syndrome. Another, in Cancer Discovery, revealed an important pathway for the transition from a pre-leukemic syndrome to AML.
These papers underscore the Crispino lab’s mission to understand the mechanisms that cause progression from pre-leukemic syndromes. The team’s ultimate goal is to either prevent progression or better treat patients who've already progressed.
A new target for Down syndrome leukemia
Down syndrome occurs when a child is born with an extra (third) copy of chromosome 21. This condition, called trisomy 21, predisposes children with Down syndrome to leukemia, particularly B cell acute lymphoblastic leukemia (B-ALL). However, the genes on chromosome 21 that contribute to cancer are not well understood.
DYRK1A is a serine/threonine kinase encoded on chromosome 21 that is implicated in several aspects of Down syndrome, including cognitive deficits and Alzheimer’s disease. In a recent paper, published in the Journal of Clinical Investigation, Crispino and his team showed that DYRK1A contributes to B-ALL by controlling transcription factors called FOXO1 and STAT3.
The researchers showed by genetic and pharmacologic inhibition of DYRK1A, they could decrease leukemic cell expansion and suppress B-ALL development in cells and mouse models. This work reveals a DYRK1A/FOXO1/STAT3 axis that facilitates the development and maintenance of B-ALL.
“DYRK1A is a therapeutic target in B-cell leukemia,” says Crispino. “And it turns out, it's actually not just in Down syndrome cases. We think it's also in other high-risk cases of B-cell leukemia.”
Understanding what drives myelofibrosis
Myeloproliferative neoplasms are a collection of diseases that can affect children but, more commonly occur in people as they age. There are three subtypes of myeloproliferative neoplasm, the worst of which is called myelofibrosis. Patients with myelofibrosis have a 20% risk of developing aggressive AML, with an average life expectancy of under five months.
Crispino and his team recently set out to understand the pathways that promote progression, from myelofibrosis to AML. In a study presented as a plenary lecture at the American Society of Hematology annual meeting in December 2020 and published in Cancer Discovery, the researchers revealed one such pathway.
Using CRISPR genetic screening, the researchers looked for tumor suppressors that when dialed down or missing would promote this leukemic progression.
“At the end of the day, we settled on one gene,” says Crispino. “The name of the gene is STK11, which encodes a protein named LKB1. LKB1 is a well-known tumor suppressor in solid cancers, but it had not been identified as a tumor suppressor in blood cancer before our work.”
The research spans from a very basic CRISPR screen with a mouse model all the way through the genetics in human patients. The researchers are following up with pre-clinical studies for a drug that affects this pathway. This drug is already in clinical trials for a type of kidney cancer.
Looking ahead: Taking on the big questions
Now that Crispino’s lab is up and running at St. Jude, he says he’s looking forward to new collaborations. This is paired with St. Jude resources for creating and studying mouse models and conducting large screens with CRISPR technology, which are helping to propel the lab’s work.
Going forward the lab will tackle big questions, such as what are the common pathways that promote the progression of these different pre-leukemic disorders? They will also be looking at the differences between these disorders in children and adults.
“It’s really about trying to prevent leukemic progression in people,” says Crispino. “We’ll be using that same CRISPR screening approach to look at the progression in a variety of blood disorders.”






