St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
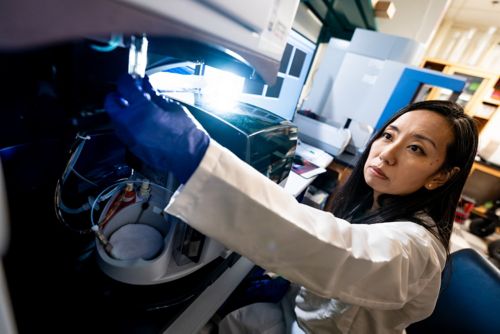
Masayuki Yamashita Lab
Decoding cell death programs in hematopoietic stem cells to understand blood disorders
About the Yamashita lab
Hematological disorders often arise from the emergence and accumulation of abnormal hematopoietic stem cells (HSCs). Our laboratory is interested in how these abnormal stem cells develop from normal counterparts. We explore molecular mechanisms that regulate HSC survival versus elimination and how they go awry during disease development. Our work provides us with potential targetable vulnerabilities that could be translated into the next generation of clinical therapies.

Our research summary
HSCs are rare, multipotent stem cells that differentiate into blood and immune cells. These self-renewing cells spend most of their time in quiescence. They can withstand cellular stresses that typically kill other types of cells, which allows them to survive and regenerate the entire blood system in response to infection, chemotherapy and transplantation.
HSCs have a propensity to accumulate mutations due to low-fidelity DNA repair mechanisms. These mutations serve as the genetic foundation for malignant hematological disorders such as leukemia and lymphoma, as well as non-malignant hematological disease such as aplastic anemia and paroxysmal nocturnal hemoglobinuria. Therefore, it is imperative that HSCs quickly discard damaged or mutated cells while preserving healthy cells. However, we lack a comprehensive understanding of how HSC survival and elimination are regulated.
Our laboratory focuses on decoding the molecular mechanisms behind HSC survival and elimination and identifying molecular targets of HSCs that could be used to prevent or treat blood disorders.
Programmed cell death
Unhealthy or unwanted cells can be eliminated through programmed cell death (PCD) pathways. These pathways are activated in response to intrinsic and extrinsic stressors such as DNA damage and inflammation. These signals trigger an intracellular proteolytic or phosphorylation cascade which, depending on the type of cell death, results in either membrane blebbing and DNA fragmentation or cellular rupture.
HSCs express PCD molecules but, compared to other cell types, have a unique response to stressors that typically activate PCD pathways. We are interested in better understanding the role of cell death molecules in stem cell regulation. PCD can cause cellular consequences other than killing the cell. Therefore, it is possible that these molecules have functions outside of cell death in HSCs and could contribute to cellular processes such as differentiation.
Specifically, we are interested in the cell death-independent effects of necroptosis on HSC aging and age-related hematological disorders. Our work has shown that MLKL, a necroptosis effector, plays a pivotal role in HSC aging and highlights the potential of targeting necroptosis molecules to prevent HSC aging.
HSC clearance by adaptive immunity
HSCs are long-lived and prone to produce mutated clones. Typically, the adaptive immune system presents non-self antigens, such as those arising from aberrant HSC clones, on MHC class-I molecules to facilitate their recognition and clearance by cytotoxic T cells. However, we are still trying to understand how HSCs and T cells interact with one another. Some stem cells are not subject to immune clearance, but the exact molecular underpinning of this evasion is not well understood for HSCs.
We are striving to dissect the interplay between HSCs and T cells. Our laboratory has shown that HSCs are highly susceptible to T cell-mediated killing compared to other progenitors, and we aim to determine exactly how this is occurring on a molecular level. We are also interested in what happens when this goes awry.
This work stands to reveal T cell-mediated control of HSC integrity and provides a foundation for future studies that use antigen-specific T cells to kill HSC clones with tumor-relevant mutations.

Publications
Contact us
Masayuki Yamashita, MD, PhD
Assistant Member, St. Jude Faculty
Department of Hematology
MS 355, D3021.01
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS