St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
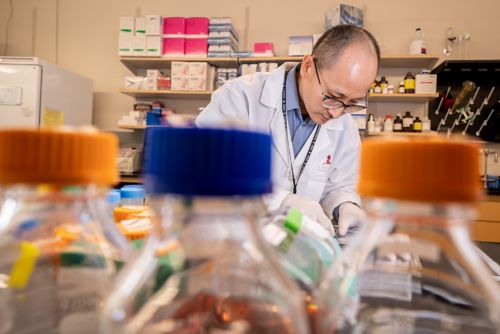
Myriam Labelle Lab
Studying how components of the microenvironment, particularly blood platelets, immune cells, and the extracellular matrix, contribute to cancer metastasis
About the Labelle Lab
Metastasis, the spread of cancer cells from the primary tumor to other sites within the body, accounts for ninety percent of cancer-related deaths. To develop effective therapies to treat metastatic cancer, it is critical to increase our basic understanding of the molecular mechanisms driving metastasis. That is our laboratory’s primary goal, and we focus our efforts on examining how interactions between cancer cells and components of the microenvironment—blood platelets, immune cells, and the extracellular matrix—impinge on cancer progression and metastasis.
Our research summary
Metastasis causes the vast majority of cancer deaths. Metastasis occurs when malignant cancer cells succeed in completing the metastatic cascade—an invasion of surrounding tissues, transit through the blood circulation, arrest and survival in distant organs, and metastatic outgrowth.
One important regulator of malignant progression and metastasis is the dynamic crosstalk between tumor cells and their microenvironment. For instance, blood platelets and immune cells interact with cancer cells during transit through the bloodstream and play crucial roles in supporting the metastatic dissemination of cancer cells.
However, the molecular mechanisms by which these host cells interact and communicate with each other and tumor cells—and how these interactions are regulated—remain largely unknown. The goals of our research are to elucidate these important cellular interactions and to determine how we could target them pharmacologically to limit cancer metastasis.
How do platelets increase the metastatic potential of tumor cells?
One of our main goals is to identify key molecular pathways triggered by platelets in tumor cells and to determine whether these alterations play functional roles in metastasis. Furthermore, we are interested in the following questions: Do cancer cells from different tissues of origin, or with different metastatic potentials, respond differently to platelet-derived signals? Are platelet-induced gene expression changes predictive of the metastatic potential of tumor cells? How do anti-platelet treatments impact specific steps of the metastatic cascade? To address these questions, we develop innovative in vitro and in vivo models and leverage advanced imaging technologies and next-generation sequencing approaches.

How do platelet-immune cell interactions impact cancer progression and metastasis?
Our previous work demonstrates that platelets and granulocytes interact with tumor cells in the bloodstream and form signaling microenvironments (termed “early metastatic niches”), which are necessary for efficient metastasis. To follow up on these findings, we investigate how platelet-immune cell interactions are modulated during cancer progression and how this specifically impinges on the efficiency of the different steps of the metastatic cascade.

How is collagen linearization regulated during cancer metastasis?
While studying platelet-tumor cell interactions and their downstream effectors, we made the exciting discovery that WISP1 (CCN4), a secreted protein expressed in metastatic tumor cells, promotes collagen linearization by a mechanism that is independent of cell-generated mechanical forces. Collagen linearization correlates with progression to metastatic disease and poor outcome in breast cancer patients. However, the mechanisms responsible for collagen linearization are not fully understood.
Current projects in the lab aim at elucidating the molecular mechanisms involved in WISP1-collagen interactions and how additional secreted factors such as WISP2 (CCN5) modulate these mechanisms. Our ongoing studies also test the functional involvement of WISP1 and WISP2 in breast cancer and osteosarcoma and how they could be targeted to treat or prevent metastatic cancer.
Our research program is unique in the way it bridges the fields of basic platelet and immune cell biology and cancer metastasis biology. This specific area of research has received limited attention but has the potential to identify valuable therapeutic targets to prevent the formation of clinically relevant metastases.
Publications
Contact us
Myriam Labelle, PhD
Associate Member
Division of Molecular Oncology
Department of Oncology
MS 354, Room D5024G
St. Jude Children's Research Hospital
Memphis, TN, 38105-3678 USA GET DIRECTIONS