St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Asunción Mejías, MD, PhD, MsCS
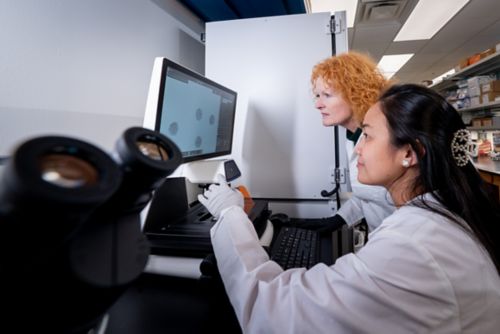
Characterizing the immune response to viral respiratory infections such as RSV, understanding the impact of coinfections, identifying host factors that predispose to severe disease and developing age-targeted interventions.
Overview
Respiratory syncytial virus (RSV) is the leading cause of hospitalization in infants worldwide and is associated with severe disease in immunocompromised children. While we currently have preventive strategies targeted to young infants, we lack effective preventative measures for a large proportion of our pediatric population. Our group is focused on understanding the interplay between RSV and the host immune system and studying the impact of viral and bacterial coinfections on this highly dynamic relationship. This approach allows us to identify those at higher risk for disease, to understand how RSV can lead to long term sequelae and to develop novel preventative strategies.
Mejías Research Summary

RSV is the leading cause of viral lower respiratory tract infections (LRTIs) in infants and young children. In addition to causing millions of hospitalizations, RSV-induced LRTIs, such as bronchiolitis and pneumonia, are the causative agents for approximately 100,000 deaths annually. Despite the recent development of effective RSV immunizations for young infants, such as extended half-life monoclonal antibodies and a maternal vaccination, the burden of RSV remains high and the clinical approach to RSV remains largely supportive and preventative.
RSV is a challenge as its course of disease has proven paradoxical compared to other viruses. Care teams need novel strategies to alleviate the burden of this disease. Our work, in parallel with the Ramilo lab, provides an essential framework for understanding RSV and its impact on the immune system.
Understanding the host response to infection
RSV is especially dangerous for young infants and is associated with significant morbidity, but RSV also impacts older pediatric age groups and immunocompromised children. Prognosis is often determined by the host’s antiviral response as well as the proinflammatory systemic and mucosal immune responses. These responses can be influenced by many factors including, but not limited to, age and the presence of bacterial and/or viral coinfections.
Age is more than a number
Age is a relevant risk factor for RSV. Infants less than six months of age have an undeveloped interferon response which, in turn, impacts B cell responses and the ability to generate an efficient protective antibody response when infected with RSV. The recent development of monoclonal antibodies and maternal vaccination provides this vulnerable population with protection during a time when they cannot generate a robust immune response on their own. However, there is still a need for effective preventative measures for older infants and children, including those that are immunocompromised.
For example, after the COVID-19 pandemic, we observed an increase in the average age of children hospitalized with RSV infection as well as more severe disease in infants, compared to pre-pandemic years. Data from after the COVID-19 pandemic also showed that the proportion of RSV/viral coinfections was substantially higher compared to pre-pandemic. These findings highlight the need to focus on and develop vaccines for older pediatric age groups.
We have also identified age-dependent mucosal and systemic interferon and antibody responses that correlate with disease severity. A better understanding of the dynamics between RSV and the host immune system in all pediatric age groups is crucial to advancing our standard of care and developing prevention strategies for the most vulnerable.
The impact of coinfections
New evidence suggests that clinical outcomes for children with RSV are also impacted by the presence of other pathogens. We are interested in characterizing the combinatorial effect of bacterial and viral coinfections on the immune response and on clinical disease severity.
Work in this space has already demonstrated that the combination of RSV with S. pneumoniae or Hemophilus induces a unique, pro-inflammatory innate immune response that is linked to worse clinical outcomes. Respiratory viruses such as coronaviruses, rhinovirus, metapneumovirus and parainfluenza viruses are often co-detected with RSV and must be studied if we are to improve clinical outcomes.
Selected Publications
Contact us
Asunción Mejías, MD, PhD, MsCS
Member, St. Jude Faculty
Department of Infectious Diseases
MS 320, Room E8053
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS


