St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
The body has checks and balances. A misaligned system can often be rescued by a related protein or the up- or down-regulation of alternative pathways. To find the chain of events that causes disease, the layers of effect must be peeled back, piece by piece.
HNRNPH2 mutations have been found in over 30 individuals with traits of neurodevelopmental disorders, such as intellectual disability, developmental delay, and autism spectrum disorder. The gene encodes a specific protein within a group called the heterogenous nuclear ribonucleoprotein (hnRNP) family. These hnRNPs are pivotal to many processes tied to RNA handling, including transcription and translation.
In a study published in the Journal of Clinical Investigation, co-corresponding authors Hong Joo Kim, PhD, Department of Cell & Molecular Biology, and J. Paul Taylor, MD, PhD, Executive Vice President, Scientific Director, and Department of Cell & Molecular Biology chair, uncovered the role that the protein hnRNPH2 (H2) plays in neurodevelopmental disorders, shedding light on the mechanisms underlying its pathogenicity. The work provides critical insight into the biology of this poorly understood disorder, with the potential to develop future therapeutics that target this and related mechanisms.
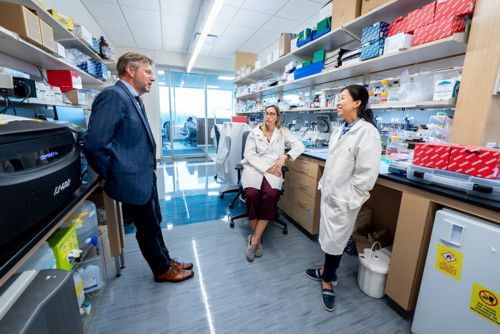
Co-corresponding author J. Paul Taylor, MD, PhD, Executive Vice President and Scientific Director, discusses research with first author Ane Korff, PhD, and co-corresponding author Hong Joo Kim, PhD, both of the Department of Cell & Molecular Biology.
“The findings from this study represent crucial documentation on the path to introducing a therapy for children with mutations in HNRNPH2,” Taylor said. “It’s an essential pre-clinical step.”
Most HNRNPH2 mutations are found within or adjacent to H2’s nuclear localization signal, which acts as the protein’s security clearance to enter and exit the nucleus. Considering that H2’s function is vital to RNA processing, mutations affecting its nuclear localization signal are significant because they can cause the protein to become stranded outside the nucleus. However, detailed mechanistic insight has been elusive due to a lack of robust disease models.
When the researchers evaluated the pathogenic form of H2 containing a mutated nuclear localization signal, they saw that access to the nucleus had been reduced. The team dug deeper using mouse models and human cell lines either completely lacking HNRNPH2 or containing the disease-causing mutation. Mice with mutated H2 showed signs of the disorder, demonstrating that the researchers successfully created a faithful disease model.
Surprisingly, mice lacking the murine homolog Hnrnph2 showed no detectable phenotypes, indicating that this was not a simple case of loss of function. The team examined the expression patterns of other hnRNP family members to identify any correlations. One stood out: hnRNPH1 (H1), a protein functionally related to H2. The researchers found elevated H1 levels in mice and human cells lacking H2, suggesting that H1 can compensate for the complete loss of H2 and act as a fail-safe to rescue the affected cells. However, while the loss of H2 can trigger compensation by H1, the disease-causing mutated form of H2 does not.
These fundamental genetic insights identified a strategy for therapeutic intervention using antisense oligonucleotides (ASOs), synthetic RNA molecules designed to bind to naturally occurring messenger RNA. ASOs have been used to successfully treat spinal muscular atrophy and hnRNPH2-related disorders. The compensatory relation between H1 and H2 suggests that one could design an ASO aimed at reducing the levels of H2, thereby inducing an upregulation of H1 to compensate for the loss of H2 function.