St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Many infectious and inflammatory diseases, including malaria, COVID-19, and sickle cell disease, cause red blood cells to rupture, releasing the oxygen-binding molecule hemoglobin in a process called hemolysis. The hemoglobin then breaks down in the bloodstream, releasing a substance called heme. Circulating heme can cause significant inflammation and organ damage, leading to morbidity and mortality.
In a paper published in Cell, St. Jude researchers reported their discovery that the NLRP12 protein, an innate immune pattern recognition receptor, is the key molecule driving heme-induced inflammatory cell death. However, heme alone is insufficient to induce NLRP12 expression and the subsequent cell death process.
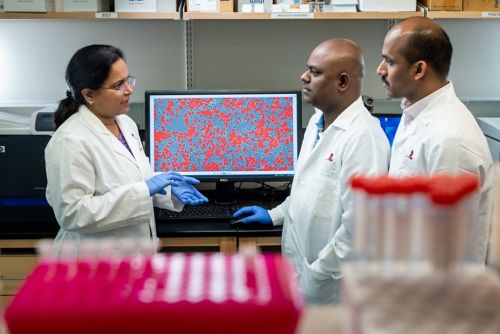
Corresponding author Thirumala-Devi Kanneganti, PhD, and co-first authors Balamurugan Sundaram, PhD, and Nagakannan Pandian, PhD, showed how NLRP12 connects hemolysis to inflammatory disease.
“After a two-decades-long search for the trigger of NLRP12 and the specific signaling pathway it activated, we found that heme, combined with specific components of infection or cellular damage, can activate NLRP12 to drive inflammatory cell death and pathology in disease,” said corresponding author Thirumala-Devi Kanneganti, PhD, Department of Immunology vice chair and Center of Excellence for Innate Immunity and Inflammation director.
The researchers showed that cell death can occur when heme combines with certain pathogen-associated molecular patterns (PAMPs) or cytokines. These combinations are common during infections and disease. When present, they signal the cell, causing NLRP12 to interact with other proteins. These interactions enable NLRP12 to form a PANoptosome, a complex comprising several cell death–inducing molecules, including the NLRP3 inflammasome, caspase-8, and RIPK3. These components are central to inducing PANoptosis, a form of innate immune inflammatory cell death, and inflammation downstream of NLRP12 activation.
Overactivation of PANoptosis leads to inflammatory disease. Therefore, NLRP12 is a direct bridge from hemolysis to inflammatory disease.
The team found that NLRP12 is expressed highly in patients with various diseases, including diseases with a prominent hemolytic component, such as sickle cell disease and malaria, and infections, such as COVID-19, influenza, and bacterial pneumonia. When the researchers knocked out Nlrp12 in a mouse model of hemolytic disease, the mice no longer succumbed. This work demonstrated that NLRP12-mediated PANoptosis is a key driver of morbidity and mortality. The results also identified NLRP12 as a potential drug target to block tissue damage, pathology, and mortality during hemolysis.
“Beyond the fundamental contribution to the innate immunity and cell death fields, this study identifies a druggable target to directly reduce the organ-damaging inflammation caused by infection and hemolytic diseases,” said Kanneganti.
The results’ implications are important in hemolytic disease and extend to infections and other conditions in which hemolysis occurs. Research has linked genetic mutations in NLRP12 to several diseases. Now that NLRP12’s regulation and function in inflammatory cell death have been identified, scientists can develop potential therapies to prevent cell death and inflammation in diseases. Additionally, these findings lay the foundation for new research on PANoptosomes and PANoptosis in health and disease.