St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Histology detectives magnify the clinical and research mission of St. Jude
Scientists at St. Jude use histology to help make accurate diagnoses that impact patient care.
Imagine a child arriving at the hospital, and their parents and doctor worry that they might be sick with cancer. It’s time to call in the cancer detectives: specialists who can determine what kind of tumor or blood disease is making the child sick. Like the detectives you see on television or read about in books, these specialists use many tools to solve the mystery.
Depending on the doctor’s concerns, the process starts with imaging or blood work to determine whether a tumor is causing problems or if something is wrong with the cells in the blood. The cancer detectives use histology as their next step to catch the cancer culprit. Like a detective’s magnifying glass, histology is a useful tool to comb the crime scene for evidence.
Histology: A key tool in the cancer detective toolkit
Histology is a test wherein tissue is analyzed by looking at it under a microscope. To perform the test, the histology team carefully cuts a tissue sample into small pieces, adding staining agents to thin tissue sections that pick up certain cell features. Medical specialists called pathologists study the sample using a microscope.
The most used stains in the histology laboratory are hematoxylin and eosin, H&E for short. H&E stains tissue in different shades and textures of pink and purple. Pathologists can interpret the cells’ arrangement, size and color to identify the tissue, decide whether it’s cancer, and, if so, diagnose the type. In many cases, as with seeing incriminating fingerprints at a crime scene using a magnifying glass, pathologists can identify the child’s disease just by looking at the tissue with an H&E stain. For example, blood cancers such as leukemia, a cancer of white blood cells called a lymphoma or a soft tissue cancer called a sarcoma are all readily identifiable by histology.
In some cases, more information is needed than the H&E stain can provide, so pathologists also use additional stains that recognize specific proteins. This process is like using a special ultraviolet light to look for crime scene clues instead of just the magnifying glass. For example, the pathologist can look at an H&E-stained slide and decide that the tissue belongs to the general sarcoma category. But there are several types of sarcoma, and to make an accurate diagnosis, the pathologist needs to know what kind. Staining for proteins found in specific types of sarcoma can help solve this mystery.
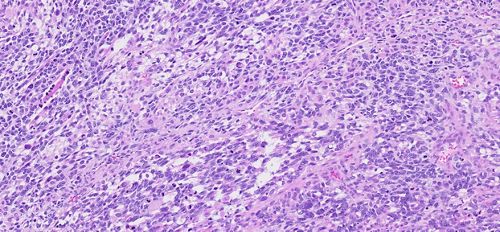
The most used histology stains, hematoxylin and eosin, turn tissue shades of pink and purple enabling pathologists to interpret what the tissue looks like.
Oncologists need this information to determine which type of treatment suits their patient because different cancers respond best to different treatments. Enrollment on a St. Jude clinical trial for patients with a specific type of sarcoma called rhabdomyosarcoma requires a diagnosis based on histology. Pathologists can get even more specific, figuring out the type of rhabdomyosarcoma and then identifying unique molecular changes in that particular cancer. This process provides guidance, determining which treatment the patient needs.
In a recent study published in Neuro-Oncology, Jason Chiang, MD, PhD, St. Jude Department of Pathology, and neuropathologist colleagues at St. Jude found combining analysis of histology and molecular features generates the most informative diagnosis for risk stratification and therapy selection in young patients with a specific type of brain cancer called high-grade glioma.
Adding more complexity to the histology toolkit
St. Jude has pioneered using large genomic studies to understand childhood cancer better and improve diagnosis. This work helps doctors find the best treatment for these rare and devastating diseases. Before this special testing occurs, however, histology is still needed to ensure that the tissue sample going through sequencing is cancer tissue and has enough cancer cells for the analysis. Otherwise, it might not be possible to identify the molecular changes in the cancer because the tissue could be full of normal cells. The clues obtained from combining histology and molecular changes help provide a complete picture of the cancer culprit. The correlation of histology, genetic findings and additional testing form the foundation of groundbreaking, comprehensive data-sharing initiatives at St. Jude, such as the Childhood Solid Tumor Network.
Innovations in experimental techniques bring new approaches to understanding cancer biology. For example, spatial transcriptomics enables researchers to find out where in a cancer and in what cell types different genes are expressed. Pathologists look at the tissue on a slide and see where the cancer is, what is around the tumor, and what proteins the tumor and its neighbors express. Spatial transcriptomics does the same but examines gene expression rather than protein expression and analyzes hundreds or thousands of genes instead of a handful of proteins. Histology chooses the right tissue to study and ensures that spatial transcriptomics’ complex gene expression profiles make sense. In the detective’s arsenal, spatial transcriptomics adds much greater magnification and a blacklight to the magnifying glass. For example, in Nature Communications, St. Jude researchers recently used histology and spatial transcriptomics to understand the biology of mouse models of liver cancer hepatoblastoma.
St. Jude employs and has pioneered many investigative tools to understand childhood cancer better. But cancer diagnosis still starts with histology: the trusty magnifying glass of the detective’s toolkit. In the laboratory, histology continues to help solve the cancer whodunit.