St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Why are we still studying COVID-19?

SARS-CoV-2, the virus that causes COVID-19, is still circulating within the population. Researchers are working to understand what this means long-term
They say that time heals all wounds. But it also reduces the intensity of our empathy for others. In many ways, the COVID-19 pandemic, with masking, social distancing and sanitizing, is over. But COVID-19 is not a relic of the past or a societal point in time. SARS-CoV-2, which causes COVID-19, is a contagious and potentially deadly virus that evolves rapidly, the long-term implications of which are still being uncovered.
The welcome introduction of vaccines has brought with it a sense of confidence and ease that has allowed many to place a capstone on the pandemic: 2020-2023. However, many other people, from the immunocompromised to those still ill with long COVID, continue to have their lives upended by the virus. The very public fight against this new pathogen that dominated life pre-vaccine has receded into the laboratory, where scientists and clinicians are still at work. Why are we still studying COVID-19? Because there is still so much value to gain from research into SARS-CoV-2 and the immune system.
At St. Jude, scientists have been studying the virus since before it even arrived in the institution’s hometown, Memphis, Tennessee, generating an invaluable cohort for scientific study and the potential for compelling discoveries to be made.
Preventing infection and learning on the way
St. Jude has been a World Health Organization (WHO) Collaborating Center for Influenza for almost 50 years. This positioning has made the hospital a leading voice on zoonotic (animal-born) viruses, including SARS-CoV-2. Indeed, before the virus had even reached Memphis, the hospital set up a screening protocol to track the virus and prevent transmission to employees and patients. This presented an opportunity to investigate how our immune systems combat infection from the first encounter. The St. Jude Tracking Study of Immune Responses Associated with COVID-19 (SJTRC) enrolled employees at St. Jude who volunteered to participate in the research at the very start of the pandemic.
“We had everyone pretty much enrolled before COVID came to Memphis, and so we have true baselines,” said Paul Thomas, PhD, St. Jude Department of Host-Microbe Interactions and principal investigator in SJTRC. Thomas has been involved in this study from the start.
“It was a particularly well-defined cohort because we had weekly testing being done here,” he explained. “So, we caught people very early in their infections, often before they knew they were infected.”
Why do some not get sick?
SJTRC is ongoing, with a subset of the original cohort asked to give samples regularly. The large sample size and rigorous resampling allow Thomas and his colleagues to get at some pressing issues still surrounding the virus. “There are people that don’t think they’ve ever had it. One of the things we can ask is whether that is true.”
The resilience of people who never caught COVID-19 but have undoubtedly been exposed lies in their immune response. What makes them special?
“Using that cohort in particular is the ideal opportunity for us to rigorously define what that T-cell [immune-cell] response to an infection looks like across the human population,” Thomas said, “and how that matures with time and relates to protection.”
Recent work from Thomas’s lab appearing in Cell highlighted the importance of T-cell response in the context of the mRNA vaccine produced to combat SARS-CoV-2.
“We’ve started seeing more and more convincing data indicating that T cells play a key role in limiting severe disease and death,” he said, but is hesitant to put all the onus on them. “There’s just so much work to do to get to the point where we can say, ‘These are the parts of your immune response that are needed to fight infection.’ Figuring out that sort of combination menu is difficult.”
Understanding the immune response is only one side of the coin. On the other side are the evolutionary forces that drive a virus to undo or circumvent the immune system’s work. Currently, researchers have found themselves in a molecular stand-off. Viruses like SARS-CoV-2 exist not as one entity but as multiple variants, each with its own unique traits.
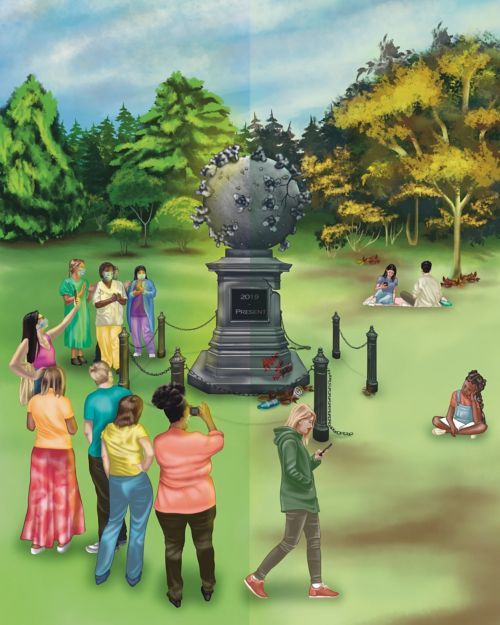
At its onset, COVID-19 was regarded by the world with reverence and measured concern. Through the drone of daily life and new routines, the way many people view this topic has now dulled. The above illustration is a reflective piece on the evolution of this public thought, and hopefully refocuses our attentions back to curiosity, health, and protection. Artwork by AnnElizabeth White.
The family business: Viral evolution
The evolution of a virus can be traced using a family tree. These “phylogenetic” trees show each virus variant’s branches, lineages, and timelines, allowing scientists to explore the rationale behind their development. The reason a seasonal flu vaccine can be offered is because each variant’s lineage is relatively straightforward.
SARS-CoV-2, from an evolutionary perspective, follows the beat of its own drum.
Richard Webby, PhD, St. Jude Department of Host-Microbe Interactions and Director of the WHO Collaborating Centre for Studies on the Ecology of Influenza in Animals and Birds, has found a home teasing out the method from the madness.
“[With flu], something a bit novel that offers an advantage will come up, and old ones will all go away,” he explained. “All the movement goes down one branch.”
SARS-CoV-2 does not follow this linearity. Multiple variants can exist within a population simultaneously, mutate, die down, move to a different host and then come back, all based on environmental pressures.
“You get the same sort of thing [as flu], evolution down one branch,” Webby said. “But then suddenly, the next variant comes from somewhere way back in the phylogenetic tree. The question is, ‘Where is that coming from?’ There’s got to be a source.”
A unique opportunity to evolve
The ability of SARS-CoV-2 to move between some animals with relative ease may explain this propensity to evolve unpredictably. While influenza viruses can also enter new host species (consider swine or bird flu), it is a rare occurrence for the virus to jump into humans. As viruses evolve differently depending on the host, the potential for SARS-CoV-2 to jump from animals into humans has researchers on high alert.
A recent study from The Ohio State University College of Veterinary Medicine and National Institutes of Health, to which Webby contributed, explored this phenomenon in white-tailed deer. The researchers found that the evolution of SARS-CoV-2 is three times faster in deer than in humans. Additionally, the pressures that drive this evolution differ from those observed in humans.
“The immune pressures are different; a deer population is probably not exposed as often to SARS-CoV-2,” Webby said. “Their immune pressure is not driving change or is driving it in a different direction than what we’re seeing in humans.” He also indicated that the longer a virus circulates in a host population, the better it navigates this unique environment. “It has to interact with different host machinery in a deer cell as opposed to a human cell, and that can make the virus adapt in different ways.”
The swift evolution of the virus in other hosts increases the chance for it to jump back to humans as a new variant. The long-term implications of this are yet to be seen, but the researchers stress that the most likely outcome is that the virus clusters circulating through the deer population will die off and not pose a risk to humans.
There are other reasons SARS-CoV-2 demonstrates such unpredictable evolutionary behaviors. On the flip side of those who are exposed to SARS-CoV-2 and do not get COVID-19 are those who are immunocompromised and struggle to clear the virus.
“They don’t have the same amount of energy to clear the virus,” Webby explained. “The virus replicates for a longer period. The more a virus replicates, the more mutations it makes.” If an older branch of SARS-CoV-2 sits within an individual, it may return to the general population unexpectedly after seemingly dying off, with new mutations and potentially different properties from its ancestral strain.
Meanwhile, however, this individual lives under the unwavering cloud of the virus.
People may not have a good sense of where it (COVID-19) falls relative to normal life. And the truth is it’s still worse than the flu in some demographics, It’s a much more complicated virus than flu. The fundamental virology is just so much more difficult.
Living with COVID
The hard reality for individuals who experience what is called long COVID is an inconvenient truth to those who would rather move on from the pandemic. The ailment remains a puzzle, even for doctors and researchers, due in part to the complexity of the vast array of symptoms with which the condition can clinically present.
“The trouble with it is there wasn’t a simple definition for it early on, but it’s clear that it’s not one thing,” Thomas said. “The original definition was: you developed a symptom, and you still have it.”
The broadness of this net means that long COVID could manifest as extreme exhaustion, hair loss, poor concentration or any of a long list of symptoms associated with the illness. Separating it from other ailments and viruses has been tricky for researchers looking to hammer out an exact window of understanding.
While the symptoms and severity of long COVID are broad, it has been shown by numerous groups that middle-aged women and people with oxygen requirements during hospitalization stood out as most susceptible to long-term effects of COVID-19.
Thomas is hopeful such research can point to a way forward for treating long COVID. At the very least, it gives researchers a place to dig.
“We can start getting at underlying mechanisms,” he said. “There’s some that are sex-associated. There are some that are age-associated. But there are biological reasons for why these associations exist.”
COVID continues, and so must we
In 2020, humanity underwent a major shift. The general public went from knowing very little about coronaviruses to one of them consuming every facet of life. Vaccines have allowed some to return to “normalcy,” but COVID-19 is not a dot on our timeline — an event to reflect on. The virus remains in our population, and it still dominates how life is lived for many.
“People may not have a good sense of where it falls relative to normal life. And the truth is it’s still worse than the flu in some demographics,” said Thomas. “It’s a much more complicated virus than flu. The fundamental virology is just so much more difficult.”
The desire to move on should not deny the effect COVID-19 still has on the world. While it remains vital to practice reasonable care for others if we feel sick and get vaccinated, there is a clear need to understand SARS-CoV-2 better and the damage it can cause. On that front, researchers like Thomas and Webby will attest: We are still studying COVID-19 because we must.






