St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Targeting DNA damage repair gives radiation therapy a boost
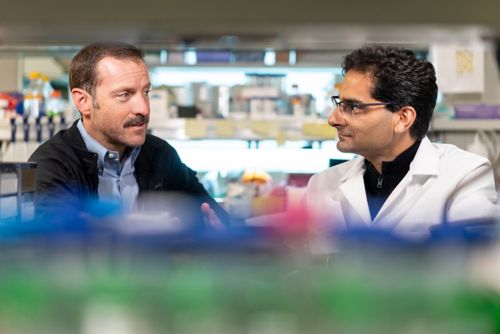
Anang Shelat, PhD, and Christopher Tinkle, MD, PhD, conducted pre-clinical studies to show how ATM inhibition can enhance the efficacy of radiation in treating high-grade gliomas.
Everyone’s DNA is constantly damaged by environmental factors, even by the process of aging. DNA damage accumulates throughout our lives, so cells contain repair mechanisms that help our bodies compensate for the damage. Cancer also causes DNA damage, but the accumulation of too much damage can kill a tumor cell, so cancer hijacks the repair mechanisms to maintain a balance that keeps it alive despite its dysfunction.
Radiation therapy triggers the accumulation of DNA damage that ultimately kills cancer cells — it is what makes it so effective. But against certain hard-to-treat tumors, such as high-grade gliomas (a type of brain tumor), additional treatments are needed.
Scientists at St. Jude are investigating combination therapy approaches, looking for compounds than can synergize with radiation therapy to make it more effective. Drug development for compounds that target DNA damage response mechanisms has exploded in the last decade, fueled by the success of drugs that inhibit a key enzyme involved in repairing DNA, PARP, in some diseases, such as ovarian cancer. Combining drugs that inhibit DNA damage repair mechanisms with radiation is a promising avenue of treatment that has a demonstrated benefit in many types of adult cancers.
Scientists at St. Jude are exploring the approach for childhood malignancies, building on over twenty years of discovery to identify novel therapeutic combinations.
DNA repair and neurological disease
In 2000, Peter McKinnon, PhD, St. Jude Center for Pediatric Neurological Disease Research chair and Department of Cell and Molecular Biology vice-chair, was studying ataxia telangiectasia (AT). AT is a rare neurodegenerative disorder that causes severe disabilities, such as difficulty with coordination and movement, a weakened immune system and a heightened risk of cancer due to a lack of DNA damage repair activity.
That year McKinnon published a study in Genes & Development, revealing the role of a protein kinase called ATM in the DNA damage repair problems observed in AT disorder. Mutations in ATM protein are the underlying cause of the disease, but McKinnon’s work helped to explain how these mutations cause AT. He found that the ATM kinase is a crucial nexus in coordinating the cellular response to DNA damage (double-stranded breaks). When those processes aren’t functioning normally, AT develops.
This work, published over two decades ago, laid the first foundational brick in a new combination therapy approach pioneered by St. Jude investigators today.
Collaboration fuels progress
Christopher Tinkle, MD, PhD, St. Jude Department of Radiation Oncology, treats pediatric high-grade gliomas, a class of particularly challenging pediatric brain tumors that is largely incurable. Research has demonstrated that these tumors have alterations in DNA damage response pathways that cause them to resist treatments, such as radiation. Tinkle and Anang Shelat, PhD, St. Jude Department of Chemical Biology & Therapeutics, whose laboratory investigates DNA damage repair mechanisms, teamed up to study DNA damage repair and radiation in these deadly brain tumors.
To do so, they collaborated with Suzanne Baker, PhD, St. Jude Department of Developmental Neurobiology. Baker studies high-grade gliomas and developed a panel of patient-derived models for studying drug response in the face of heterogeneous molecular underpinnings. That work, published in Nature Communications, was another foundational brick that led Shelat and Tinkle to their current study.
“We use patient tumor samples to develop models representing the diversity of pediatric high-grade glioma subtypes that arise in different locations and developmental stages, driven by different genetic alterations,” said Baker. “These models are critical resources for research to better understand how and why these tumors develop and to identify improved therapeutic approaches and causes of therapeutic resistance.”
Shelat highlights that adult and pediatric high-grade gliomas are very different creatures, driven by different molecular mechanisms, as part of why having pediatric-specific high-grade glioma models representing different molecular subgroups is so crucial.
“It is a great example of the collaboration and the utility of having St. Jude develop these models and make them available,” Shelat said. “Without that, our story would be very limited in its scope. But we were able to expand out and sample in these diverse backgrounds.”
For Tinkle, collaborating across disciplines was essential to finding a path forward.
“What I wanted to bring to that collaboration with Dr. Baker was to integrate radiation therapy in a clinically relevant manner so that it became part of the way preclinical studies were designed and tested,” Tinkle said. “I’m very interested in identifying agents that enhance radiation, whether through enhanced tumor growth inhibition or through more selective effects on tumors that spare normal tissue.”
Inhibiting DNA Damage Repair
Tinkle and Shelat led research, published in Neuro-Oncology, that evaluated the therapeutic potential and studied the underlying biology of combining radiation with an ATM inhibitor (AZD1390) to block DNA damage repair. AZD1390 was designed to cross the blood-brain barrier, the membrane that encapsulates the brain from the rest of the body — a significant obstacle to getting treatments to brain tumors.
The researchers used pediatric high-grade glioma cell lines in the laboratory to study the combination of ATM inhibition with radiation. They found that AZD1390 significantly increased the effect of radiation therapy across different molecular subgroups. There was some concern that the therapy may only work in cancer cells harboring mutations in TP53, which is observed in approximately one-half of pediatric high-grade glioma. But the study showed that ATM inhibition improved radiation therapy in both wild-type and mutant TP53 high-grade gliomas.
Their work supports clinical evaluation of AZD1390 in combination with radiation in pediatric patients with high-grade glioma, but the researchers aren’t stopping there. The team continues to investigate potential resistance mechanisms, particularly from germline (inherited) variants.
“One of the most important findings from our study is that this combination isn’t inducing toxicity in the brain,” Shelat said. “Radiation does have some associated toxicity, but the ATM inhibition is not affecting normal brain tissue. What we have is a good proof of concept, and it was inspired by this work from two decades earlier.”
St. Jude joins National Brain Tumor Society consortium
In 2023, Shelat, Tinkle and Stephen Mack, PhD, St. Jude Department of Developmental Neurobiology, joined the National Brain Tumor Society (NBTS) in their DNA Damage Response Consortium. The consortium launched in 2022 in a partnership between NBTS and Yale Cancer Center and has expanded to include additional partners. The consortium aims to advance potential treatments targeting DNA damage repair rapidly.
The St. Jude team combines expertise in DNA damage response, chemical biology, developmental neurobiology, drug screening and bioinformatics to focus on hard-to-treat pediatric brain tumors, including high-grade gliomas and ependymoma. The researchers plan to test drugs that inhibit several DNA damage repair mechanisms, including ATM, ATR and PARP, in addition to DNA-damaging agents such as conventional chemotherapy and radiation.
The consortium is building a core team with experience in this type of research and relationships with pharmaceutical companies to speed the development of DNA damage repair inhibitors for adult and pediatric brain tumors. The St. Jude group is the only consortium member dedicated to pediatric cancer.
Explaining the benefit of these types of collaboratives, Tinkle says, “We’ve always approached this work with translation to the clinic in mind, and you can work as hard as you can to get that, but the reality is that there are so many obstacles to that path that, even if a therapeutic approach looks good, it may not go forward. That’s why we need to partner across disciplines, to look at several different approaches in parallel, in collaboration with industry, to get the preclinical evidence that will help promising new therapeutics reach the clinic.”
Shelat added, “There are other compounds coming down the pipeline; while we’re confident in this combination [ATM and radiation], if it doesn’t pan out for some reason, there are other drugs that we can use to modulate DNA damage response.”
“Participating in this consortium allows us to share insights and collaborate within the group,” Shelat said. “But it also enables easier access to clinical candidates and will ultimately speed the development of new clinical trials for children with brain tumors.”






