St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Spilling their guts: patient microbiomes may hold the secret to predicting outcomes after transplant
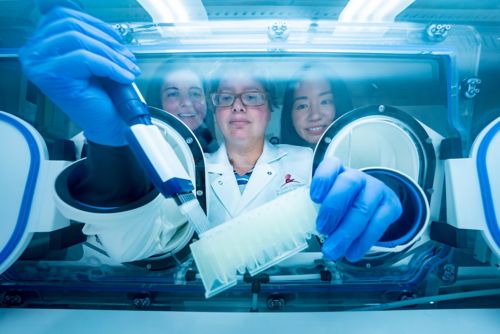
(L to R) Co-first author Gabriela M. Marón , MD, MSc, co-First and corresponding author Ellie Margolis, MD, PhD, both of St. Jude Department of Infectious Diseases, and co-author Li Tang, St. Jude Department of Biostatistics working at an anerobic hood.
Immediately after a pediatric bone marrow transplant, physicians, families and patients hold their breath for 6-8 weeks. During that time, the patient has no immune system while the transplanted blood stem cells establish themselves and start making new immune cells. Any infection is dangerous in this situation, but some patients appear more vulnerable to certain infections than others. Even after the new immune system develops, problems can arise if the newly transplanted cells fail to recognize their new home as “self.” In this condition, called acute graft versus host disease, the transplanted cells begin to attack the patient.
St. Jude infectious disease specialist Gabriela M. Marón Alfaro, MD, MSc, St. Jude Department of Infectious Diseases, became interested in understanding the interaction of the microbiome and transplant outcomes, such as opportunistic bacterial infections and graft versus host disease, through her observation of patients’ highly varied experiences of the process.
“I would see our patients come in for a transplant, and while they have all been exposed to antibiotics and hospitalizations,” said Marón, “I noticed some are colonized with antibiotic-resistant bacteria, and some are not. Why? I didn’t know.”
“And of those that are colonized, some go on to have a bloodstream infection, but not all,” she continued. “Then other patients go on to have acute graft versus host disease, leading to more infections. I wanted to understand: why this patient but not that one? Then we can develop interventions to minimize the risk of developing these diseases and improve transplant outcomes.”
In collaboration with Ellie Margolis, MD, PhD, St. Jude Department of Infectious Diseases, Marón looked at pediatric microbiomes before and after transplant in patient stool samples. They found that the bacterial signals predicting infection in adults did not translate to pediatric patients. Instead, pediatric patients have unique microbiome signatures associated with specific infections or the chance of developing other complications after a bone marrow transplant. The findings were published recently in the Journal of Infectious Diseases.
“We found four or five unique gut microbiome signals that were predictive of outcomes in children undergoing bone marrow transplant,” said Margolis. “Particular ratios of bacteria predicted if a pediatric patient was more likely to develop infections or graft versus host disease. We could see that early, before they even underwent bone marrow transplant or later, when the patient’s immune system was recovering after the transplant.”
Predicting opportunistic infections in pediatric bone marrow transplant patients
Infections during immunosuppression constitute a significant threat to patient recovery and transplant engraftment. The gut microbiome is full of bacteria that are normally a necessary part of breaking down food and other digestive functions, but after transplant, they have a chance to leak into the bloodstream while the patient’s defenses are down.
“Even though these bacteria are normally present in the gut,” Margolis said, “they are often the source of a common complication after bone marrow transplant — invasive bloodstream infections.”
“An invasive bloodstream infection is when you find bacteria in the blood that can cause sepsis, an inflammatory response that can cause poor patient outcomes and, in some cases, death,” Marón explained. “Therefore, we want to find a way to avoid them. Looking at the gut microbiota seemed like a promising place to start, based on previous literature in adults.”
In adults, the diversity of bacterial communities predicts post-transplant infection risk. This diversity is intuitive — the more types of bacteria present, the more likely one of these bacteria can keep the potentially pathogenic restrained. In addition, the presence of a specific type of bacterium, butyrate producers, independently predicts poor outcomes in adult populations. This prediction enables physicians to surveil the highest-risk patients more intensely and proactively treat them, minimizing the chance of an unchecked pathogen emerging. The St. Jude study is one of the first to evaluate whether these patterns in adults are predictive and practical in children — they aren’t.
Contrary to adults, the collaborators found that rather than the lack of diversity in bacterial communities, certain ratios of types of bacteria predicted the risk of infections in pediatric patients.
One example is an altered ratio of certain anaerobes to other gut bacteria. Anaerobes are bacteria that don’t require oxygen, making the gut an ideal home for them. They are necessary for maintaining a healthy gut ecosystem. But a combination of antibiotics, chemotherapy and disease alters the amount of these anaerobes in the gut. The researchers found if the ratio of these anaerobes compared to other gut bacterial populations becomes unbalanced, patients experienced more infections during that critical period after transplant.
The research is preliminary, but it illustrates that the makeup of the pediatric microbiome matters for post-transplant infection risk. It also shows that treatments that affect the microbiome used to prepare patients for transplant, such as antibiotics and chemotherapy, deserve some scrutiny to understand how their interactions with gut bacteria set the stage for patients’ infection risk.
While preventing infections is crucial, transplant recipients are also at risk of graft versus host disease, a severe condition that the gut microbiome can also predict.
An early warning against acute graft versus host disease
Acute graft versus host disease, a serious potential complication from bone marrow transplant, occurs when immune cells arising from the newly transplanted blood stem cells identify the patient’s original cells as foreign. When immune cells find something that is “foreign” and not “self,” they attack. This system normally works quite well, fighting off viruses and bacteria. In the case of graft versus host disease, the new immune cells start an inflammatory attack on the patient’s own tissues. The condition causes significant abdominal pain; nausea; vomiting; diarrhea; and damage to the skin, liver and gut.
Having a way to predict who is at high risk for graft versus host disease would allow physicians to prevent it or treat it sooner. The condition’s complications alone are enough to motivate physicians to intervene, but graft versus host disease also has a secondary consequence — its treatment makes patients more vulnerable to opportunistic infections.
To help better predict which patients will develop graft versus host disease, the St. Jude scientists identified two microbial signatures, one before transplant and one after, associated with later development of the condition. These included a balance (a specific ratio) of Enterobacter species to oral microbes in stool samples before transplant and a balance of lactate producers to strict anaerobes after transplant.
Interestingly, the highest association was not with a specific bacterial family or ratio of bacteria but with the presence of a bacterial metabolic pathway. The presence of arginine metabolism predicted four times the risk of graft versus host disease than any other factor. While the study did not dive into the mechanism, arginine metabolism is known to be involved in inflammatory responses, making it attractive to investigate further.
“There’s a biological plausibility to the arginine pathway being predictive because arginine interacts with our macrophages, which are sensing bacteria within our gut, and arginine can help determine how likely your macrophage is to react,” Margolis said. “I think this could be an important signal, but we’ll need to confirm it.”
Gut microbiome is a piece of the puzzle
Marón and the Margolis lab are now pursuing confirmatory experiments. They want to ensure that the connections they’ve uncovered between certain bacterial ratios, arginine metabolism, infections and graft versus host disease are replicable and consistent. During the study, patients, families, physicians and Allied Health staff partnered to participate and collect samples. They all wanted to be part of the solution, especially if it could help future patients achieve better outcomes.
Future research will require large-scale coordination of these groups at multiple institutions. Still, the initial results from this work suggest that this could be a real first step towards making clinical approaches to predict and mitigate post-transplant infections and graft versus host disease. That would let patients and their families breathe easier during that critical post-transplant period.
“These preliminary findings are very exciting,” Marón said. “If we confirm these results in a larger study, I hope to eventually take this to patient care and help us make clinical interventions. That would be the ultimate goal.”






