St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
How scientists visualize and analyze T cells

From flow cytometry to T-cell receptor specificity and cellular state, scientists at St. Jude break down the ways they study T cells.
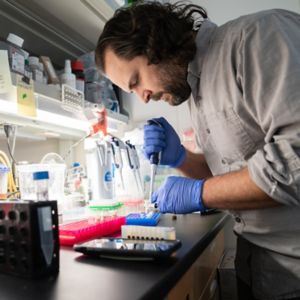
Researchers explain how the tools they use in the laboratory to study T cells work, including CoNGA a unique analysis created at St. Jude.
Welcome to St. Jude On T cells, where we’re taking a deep dive into visualizations of T cells in multi-dimensional space.
My name is Dr. Beiyun Liu, and I’m a postdoctoral researcher in the laboratory of Dr. Douglas Green at St. Jude. I will be introducing you to some methods immunologists use to understand T-cell biology.
There are many varieties of T cells: CD4+ vs. CD8+, effector vs. memory. But how did scientists figure out what they all do?
As there are countless health threats for our T cells to resist, including viruses and cancer, how did scientists figure out how T cells properly function to protect us?
Immunologists use different methods to study T cells. They are also developing new techniques to better track and analyze T cells and their function.
Making sense of T cells with flow cytometry
Scientists first saw that different immune cell types had distinct physical properties, such as size and granularity, which is the texture of a cell. To visualize these distinct properties, they used a technique called flow cytometry, where cells are forced through a narrow channel to form a stream of single cells. Then, by shining a laser beam at each individual cell, researchers were able to use how the cells deflect light to plot these cells using these two dimensions of size and granularity.
As time went by, immunologists found that in addition to physical property differences, each cell type has a unique combination of surface proteins that could be used to further identify the cells. For example, all immune cells have the surface protein marker CD45. By using a fluorescent tag or antibody that binds to CD45, then using a laser that can make it glow, we can now see that all immune cells will light up for CD45.
Scientists can identify each cell type by using a unique set of identifiers. For T cells, we can follow the entire developmental path from their beginnings in the thymus through their migration to the spleen, lymphoid organs, and peripheral blood using this set of surface protein markers.
Improving beyond flow cytometry for T-cell identification
This method works very well when we’re dealing with distinguishing markers that are on the cell surface, facing outwards from the cell. But what if the distinction lies inside the cell, or if the distinction is outside the cell, but is too small of a difference for antibodies to detect?
For example, each of our T cells expresses a unique T cell receptor, or TCR, which is what gives CD8+ T cells the ability to specifically target and kill tumor cells or infected cells. Each unique TCR can recognize and respond to only a small number of theoretically trillions of short peptide sequences. These short peptides come from recycled proteins that are chopped up inside the cell and loaded into major histocompatibility complex, or MHC, proteins that bring them to the cell surface where T cells can see them.
This is called TCR specificity, and it relies on several small regions within the TCR that are different on every cell but are too small and unique for antibodies to be able to bind. Additionally, during an active T-cell response, although we have a handful of cell surface proteins that can fluctuate on a responding T cell, vastly greater fluctuations occur within the cell involving hundreds of proteins. The complex network of interplay of these internal proteins is what fine tunes the state of the response.
Flow cytometry is limited in answering questions on both fronts. Although flow cytometry can give us a rough snapshot of whether there is a T-cell response at a given point in time, we are unable to see what occurred before this time, or to predict what could happen in the future.
To work around these hurtles, find a way to trace the history of T cell response and possibly predict future actions, scientists went back to the central dogma of cell biology, which is that DNA is transcribed into RNA, which is then translated into protein.
Since the technology is hindered at the protein level, scientists are now looking at the RNA and DNA levels. In this way, researchers seek to clarify the finer details of the trajectory of T-cell response and incorporate the aspect of time into their analysis.
Over several years, Dr. Stefan Schattgen from the laboratory of Dr. Paul Thomas at St. Jude developed a new analysis, called Clonotype Neighbor Graph Analysis, or CoNGA, to combine analysis approaches looking at TCR specificity and the T cell functional state (what it does). CONGA effectively bridges the gap between form and function.
CoNGA: A new way to analyze T cells
Immunologists have been using flow cytometry since the 1970s. At that time, we were looking at cells in terms of size and granularity, which is two dimensions. When they started incorporating fluorescent tags the dimensionality started to increase. Over the last 50 years advances in flow cytometry technology have allowed us to measure up to 60 markers simultaneously.
But now, when we switched over to gene expression data (RNA), the dimensionality crosses into the thousands as we simultaneously measure all genes expressed by the cells.
This gave us a lot of finer details on T-cell responses, but we still had an issue. For a long time, studies on TCR specificity, which asked whether a T cell can respond to a target, were done separately from those looking at the functional states of the T cells, or in other words how the T cells responded.
If we measure T-cell specificities we can tell if the patient has the capacity to respond, but by simultaneously capturing cellular state in the form of gene expression, we can tell whether or not that T cell is responding, and how. The question then become, how can we integrate these two pieces of information together to better understand if and how T cells from a patient will respond to infection or cancer.
That’s why we developed CoNGA, to link TCR specificity with cellular state.
T-cell analysis fingerprints TCRs
Think of TCR specificity as a cell’s fingerprint. While each one looks a little bit different, we can compare all the fingerprints in our collection to one another and group similar looking ones together. For example, one set might have some loops or swoops in a certain spot. Once we do this, we can then arrange all the fingerprints into a map where similar fingerprints are located close to one another in connected communities of neighbors.
The T-cell response state can be thought of as what the T cell was doing at any given point in time compared to other T cells around it. Some cells will respond similarly, and others won’t, and we can visualize the state of response in terms of neighborhoods.
If you know where a T cell is compared to other T cells on either of these neighborhoods, and then link them together, you can then confidently say if a T cell that seems like it should be responding is responding or not. For example, we can ask whether flu-specific T cells produce a robust response to the flu. We published CoNGA in Nature Biotechnology.
For now, it’s a useful tool for exploring an interpreting these high-dimensional datasets, but we’re expanding CoNGA in the hopes that it could lead us to better medical decisions and treatments down the road.
There’s a lot of scientific literature out there on how T cells are thought to function. The problem is that when you formulate hypotheses based on the literature, you’re already running the risk of biasing yourself in your experimental design and interpretation. That could lead a whole field to being stuck thinking a certain way, which may or may not actually be correct.
With CoNGA, we created an analysis pipeline that is unbiased, and could become a tool that lets the data point us in the right direction.
Images in video created using Biorender.