St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude researchers answer COVID questions

Studies led by Paul Thomas, PhD, Immunology, and Joshua Wolf, MBBS, PhD, Infectious Diseases, have helped answer questions about SARS-CoV-2.
When SARS-CoV-2 invaded the world, the virus was an unknown entity. Since early in 2020, researchers have learned a tremendous amount about the virus that caused the COVID-19 pandemic and how that virus affects the body. This includes a deeper understanding of our own immune system and how it reacts both to infection with the virus and vaccination against it.
Vaccines designed to help train the immune system to attack and defend against SARS-CoV-2 were introduced in 2021. Vaccines for those 6 months and older have helped reduce the number of deaths and serious illnesses caused by the virus. There are different types of vaccines against SARS-CoV-2, but some of the most successful and widely adopted in the US are the mRNA vaccines (Pfizer and Moderna).
While the vaccines have helped tremendously, many questions remain regarding how the immune system responds to infection and vaccination, and how these responses change as the virus continues to mutate into new variants.
At St. Jude, studies led by Paul Thomas, PhD, Immunology, and Joshua Wolf, PhD, MBBS, Infectious Diseases, continue to provide new understanding of SARS-CoV-2. Their findings have helped build the body of knowledge regarding the benefit of vaccines and when to receive them. Such knowledge plays an important role in decision making about vaccination.
Do T cells have staying power in vaccinated people?
Yes. Research from St. Jude and Washington University School of Medicine in St. Louis showed that even 6 months after vaccination, T cells targeting SARS-CoV-2 were still active in lymph nodes.
The researchers wanted to better understand the specificity and structure of the T-cell response to vaccination, so they studied T cells in the lymph nodes, which facilitate antibody development in vaccinated individuals. The scientists used samples from their collaborators and the St. Jude Tracking Study of Immune Responses Associated with COVID-19 (SJTRC). The tracking study started in 2020, enrolling St. Jude employees and monitoring their vaccination and immune response to the virus.
Different people and their T cells identify different parts of the virus, thanks in part to the variability of T-cell receptors. So, the researchers created an analysis that uses T-cell receptors to guide them to pieces of the virus that the immune system identifies most often. Called reverse epitope discovery, the analysis involves looking at clusters of highly similar T-cell receptors that recognize the virus in a similar way.
The findings, published in Cell in December 2021, showed that half of the individuals studied reacted to the same part of the virus. Furthermore, the scientists found that up to 10% of the individuals’ CD4 T cells, which help coordinate the immune response, recognized this piece. While circulating T cell responses (measured in the blood) have been shown to wane in 6 months after exposure to other pathogens, the anti-SARS-CoV-2 T cells were still present and active in the lymph nodes. Researchers also found that in the lymph nodes the T cells were often at levels matching the peak of the response (immediately following vaccination).
Importantly, the part of the virus that the T cells react to did not alter in the major SARS-CoV2 variants, including Delta and Omicron. These findings show the benefit that mRNA vaccination against SARS-CoV-2 can have over time. By focusing on T cells, the research provides optimism that the benefits will have staying power.
“A killer T cell can kill something much bigger than itself, and it can do it very fast and very subtly,” Thomas said. “The killer T cell doesn’t even break a sweat, so to speak. The next phase of vaccines against this virus will take the T cells into greater account.”
Should you get vaccinated if you already had COVID?
Yes. An individual who had a COVID infection should still get vaccinated because the vaccines will help the immune system recognize and train for additional infections by the virus. Research by Thomas, Wolf and their teams answered this question by studying how vaccination against and infection with SARS-CoV-2 affects the immune system.
Antigens are molecules that the immune system uses to recognize a threat such as an infection. Vaccinations and infections (in both the unvaccinated, considered a primary infection, and the vaccinated, considered a breakthrough infection) expose the immune system to antigens. SARS-CoV-2 variants such as Delta and Omicron also change the antigen landscape.
Researchers recently showed that while some similarities exist in the ways the immune system responds to both the vaccinated and the infected, the vaccines still provided additional stimulation for the immune response in infected individuals. Nature Immunology published these findings in April 2022. Vaccines activate and expand the immune response in ways that can be protective in individuals previously infected with SARS-CoV-2.
Even in vaccinated individuals who later get infected, the vaccine still provides protection. The vaccines target the spike protein, a part of the virus, so the immune system learns to recognize that specific viral protein. But in those who had a breakthrough infection, the diversity of their immune response increased.
“The good news story is really on the breakthrough side. It is basically like the plot of The Avengers movie,” Thomas said. “If you have a breakthrough infection and you only have T-cell memory from the spike protein from being vaccinated—like Captain America and a few of the other superheroes taking on Thanos—that won’t be enough. But if you bring in all of your non-spike memory—like when the whole Avengers team assembles or you get a breakthrough infection—you’re no longer as susceptible as you were when you were just vaccinated.”
The study used data from STJRC, which provided samples from participants before they became infected with SARS-CoV-2. This baseline was necessary to be able to draw conclusions about the impact of infection.
“Properly understanding the T-cell response to COVID-19 infection and vaccination is really challenging, but it's essential to developing a long-term control strategy for this virus,” Wolf said.
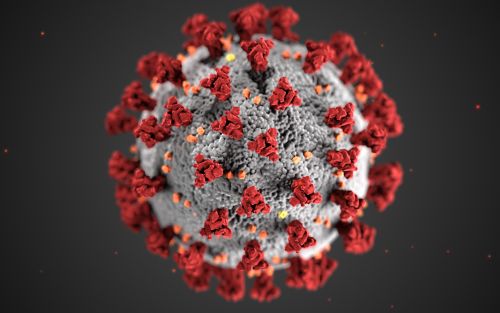
SARS-CoV-2 is the virus that caused the COVID-19 pandemic.
Should you get a booster shot of the vaccine?
Yes. Booster shots are beneficial for immune response, especially in people who are older or overweight.
Starting in the latter half of 2021, experts recommended that individuals get an additional booster shot after completing initial vaccination (2 shots of an mRNA vaccine, or 1 shot of the Johnson & Johnson vaccine). Thomas, Wolf, Stacey Schultz-Cherry, PhD, Infectious Diseases, and their teams helped shed light on how people responded to booster doses in the context of the different variants of SARS-CoV-2.
Using the SJTRC cohort, the scientists studied how antibodies against SARS-CoV-2 variants differ among individuals who were infected, those who were vaccinated and people who had breakthrough infections. The study used data from nearly 400 SJTRC participants. Of these, 120 had the infection only, 237 were vaccinated with an mRNA vaccine but never infected and 42 had a breakthrough infection after vaccination.
The researchers measured the participants’ antibody levels against the original strain of SARS-CoV-2 and the first 4 major variants to emerge (Alpha, Beta, Gamma and Delta). The Omicron variant did not yet exist at the time of the study.
Published in Clinical Infectious Diseases in January 2022, the study showed that the highest antibody levels occurred immediately after vaccination. This was especially true in individuals who were vaccinated after infection. Levels were highest against the original strain and the Alpha variant. The researchers also found that vaccinated participants had high antibody levels against the Delta variant, whereas those who had been infected only had low levels of antibodies against Delta.
In vaccinated individuals, antibody levels were highest in those who were younger, had a healthy weight or more recent vaccination. This was an expected finding similar to what has been observed from research on influenza vaccination. However, the researchers were surprised to find that in those who had been infected with SARS-CoV-2, antibody responses were highest in those who had more severe infections, poor metabolic health or were overweight, or had received the vaccination after infection. The researchers suspected that the finding was not just because the participants had more severe infections. Instead, the scientists hypothesized that higher viral load could lead to greater stimulation of B-cells or that baseline inflammation primed these individuals for antibody production.
“There has been a lot of confusion surrounding booster doses of vaccine, who should get a booster and when,” Wolf said. “A cohort like SJTRC helps provide some insight into those questions so that we can make the right recommendations about who is most likely to benefit from a booster shot.”
As the pandemic continues, so does research
SJTRC enrolled 1,316 participants who provided thousands of questionnaires, nose swabs and blood draws. Although scientists have gleaned tremendously valuable information from SJTRC, the study required a substantial commitment for participants. According to Wolf, if all 51,213 questionnaires that participants filled out were stacked on top of each other, the tower of paper would be more than 16 feet tall. SJTRC was designed to last for 1 year, but the pandemic has now stretched into multiple years.
To continue learning from this essential cohort, Wolf and his colleagues are continuing SJTRC. They are asking up to 400 prior participants to continue in the study for 2 additional years, answering surveys and providing blood and saliva samples twice a year.
“A cohort like SJTRC is so valuable for understanding what this virus is doing over time and how our bodies react to it in real time,” Wolf said. “With this extension of the SJTRC study we’ll be able to answer the next big questions that emerge, bringing us closer to ending the pandemic.”






