St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Reflecting on nearly 40 years of progress against pediatric brain tumors

St. Jude patient Charlotte Roland and her mother talk with Amar Gajjar, MD, Department of Pediatric Medicine chair.
When a child with a brain tumor arrives at St. Jude today, they have access to novel treatments and care from a multidisciplinary team of specialists who are dedicated to treating children. This might include surgery (in partnership with Le Bonheur Children’s Hospital) to remove as much of the tumor as possible and gather samples for molecular analysis in the lab. Genomic sequencing and other analyses might reveal vulnerabilities in the cancer that can be treated with targeted therapies. The patient might undergo radiotherapy developed to spare as much healthy tissue as possible. They can also enroll in a cutting-edge clinical trial designed using discoveries from the lab.
The patient experience has come a long way since the St. Jude brain tumor program launched nearly 40 years ago.
“When the brain tumor program began in 1985, we knew very little about these devastating tumors,” said Amar Gajjar, MD, Department of Pediatric Medicine chair. “Treatments were intense, and less than half of our patients survived. Those who did suffered devastating long-term effects. Since then, we have focused on defining the unique molecular make-up of brain tumors. This research is then translated into innovative clinical trials. Now, we can offer more effective, less toxic therapy which has improved survival rates.”
Today, the overall five-year survival rate for pediatric brain tumor patients is nearly 75%, but survival varies significantly based on what kind of brain tumor a patient has, and whether the tumor has spread or returned after initial therapy. Compared to the 94% survival rate for acute lymphoblastic leukemia, brain tumors lag behind. Clinical trials testing new therapies and a focus on survivorship are making a difference for patients today, while laboratory advances are continuing to highlight new ways to treat these tumors.
Innovation reveals a bright horizon
Researchers continue to look deeper into the biology of brain tumors to identify previously unappreciated weaknesses. In addition to genetics, researchers are also looking at the processes that govern how genes are expressed. Chromatin is a structure made of DNA and proteins that has to unwind to be transcribed. Transcription is the process cells use to make an RNA copy of its DNA so that proteins can be made from its instructions. The processes involved in gene expression are critical for growth and development. Researchers are learning more about how these processes contribute to brain tumors. For example, Suzanne Baker, PhD, Developmental Neurobiology, is investigating the novel oncogenic mutations that connect tumor development and chromatin regulation in high-grade gliomas such as diffuse intrinsic pontine glioma (DIPG).
St. Jude scientists are also working to identify immunotherapy approaches for pediatric brain tumors. T cells are a kind of immune cell that help fight infections and diseases such as cancer. Chimeric antigen receptor (CAR) T cells are designed to specifically target a substance (antigen) on the surface of cancer cells, while drawing immune cells to the cancer. Different types of cancer present different antigens, so finding the right one can be tricky, but CAR-T cells have the potential to be more effective and safer than conventional therapies. Giedre Krenciute, PhD, Bone Marrow Transplantation and Cellular Therapy, is leading research to develop CAR-T cell treatments for pediatric brain tumors.
Improving outcomes for cancer survivors
Treatment for a pediatric brain tumor is intense and can have lasting effects on a child’s developing brain and body. At St. Jude, researchers are dedicated to deploying technological advances and new understandings to improve brain tumor care. For example, radiation is a critical component of any treatment plan for pediatric brain tumor patients. Thomas Merchant, DO, PhD, Radiation Oncology chair, oversaw the 2015 opening of the first proton beam therapy center dedicated solely to children. Proton therapy lets doctors aim high-dose radiation at cancer cells and spare healthy cells. It is one of the most advanced and precise forms of radiation treatment and is especially beneficial for treating children with brain tumors.
Still, childhood brain tumor survivors treated with cranial radiation are at significant risk of developing cognitive late effects caused by treatment. Research by Heather Conklin, PhD, Psychology, has shown that computer-based cognitive training is as effective as medication for improving memory and attention in childhood cancer survivors with cognitive deficits. Published in Journal of Clinical Oncology, the research showed that cognitive training presented as a video game could help childhood brain tumor survivors improve their cognitive skills, including the speed at which the brain processes information.
“These results suggest that computerized cognitive training may help fill a void in management of cognitive late effects that impact quality of life for childhood cancer survivors, such as the likelihood they will complete school and live independently,” said Conklin of the 2015 study.
Another way that researchers are studying ways to improve survivors’ quality of life is through exercise. Children and adolescents who have undergone cancer treatment are often less active, may gain weight and have more health problems compared to children without cancer. Kirsten Ness, PhD, is leading ALTE1631, a web-based exercise study for children and adolescents with cancer. This study, open to brain tumor patients, evaluates the effect of a reward-based website on fitness and quality of life in children and adolescents who have completed cancer therapy.
Clinical trials bring new advances
Over the years, St. Jude investigators have focused on developing novel clinical trials for both newly diagnosed and relapsed pediatric brain tumor patients. One example is SJMB03, an international, multicenter phase 3 clinical trial for children with newly diagnosed medulloblastoma. The study ran from 2003–13 and provided risk-adapted therapy based on the clinical features of the tumor. The study confirmed the frequency and clinical significance of molecular groups and genetic alterations using DNA methylation and next-generation sequencing. The results were published in 2021 in the Journal of Clinical Oncology and informed the design of the next medulloblastoma clinical trial, SJMB12. The first clinical trial to treat newly diagnosed medulloblastoma patients based on their molecular group, SJMB12 will be completed this year.
St. Jude also participates in large, national and international efforts to study pediatric brain tumors. For example, Merchant led a study through the Children’s Oncology Group (COG) that evaluated treatment for ependymoma. Published in 2019 in the Journal of Clinical Oncology, this was the first cooperative group study to give immediate postoperative radiation to children under age 3 with ependymoma. The results showed that administering radiation right away after surgery nearly tripled survival.
Over the years, St. Jude has also been a key collaborator in the Pediatric Brain Tumor Consortium (PBTC). PBTC was founded in 1999 to improve the treatment of primary brain tumors in children. Since then, St. Jude has led the operations, biostatistics and data management core of PBTC. Under the direction of Arzu Onar-Thomas, PhD, Biostatistics, St. Jude collaborates with investigators from 15 academic centers and hospitals across the U.S. and Canada to develop superior treatment strategies for pediatric brain tumors.
Increasing understanding of brain tumor biology
Scientists at St. Jude took some of the earliest steps in defining the molecular and genetic basis of brain tumors. The Pediatric Cancer Genome Project (PCGP) was a three-year effort by St. Jude and Washington University School of Medicine to sequence the complete normal and cancer genomes of 800 pediatric cancer patients. The PCGP defined the molecular basis of pediatric cancer including brain tumors.
Discovering genetic mutations, altered signaling pathways and dysfunctional proteins facilitated the development of preclinical models of disease and accelerated the clinical pipeline. For example, Martine F. Roussel, PhD, Tumor Cell Biology, conducts pre-clinical research which helps guide the clinical development of new treatments based on biologic findings.
“This type of research can help span the gap between basic discovery and clinical use, which can take years,” Roussel said. “We create faithful and accurate laboratory models to investigate how the molecular factors within tumor cells interact with, and respond to, different treatments. It is very gratifying to see discoveries that define and instruct pre-clinical trials transition into the clinic where they will hopefully benefit patients.”
Recently, Roussel’s work identified a class of drugs called CDK4/6 inhibitors as potentially useful. Based on her findings, investigators at St. Jude decided to incorporate CDK4/6 inhibitors into a clinical trial called SJDAWN. Giles Robinson, MD, leads SJDAWN, which is a phase I clinical trial offering combination therapy for patients with medulloblastoma and ependymoma. The trial has three arms, each testing the CDK4/6 inhibitor ribociclib paired with another drug.
Molecular diagnostics guide clinical care
The ability to study clinical samples from different types of brain tumors has led to a much more detailed understanding of the biology that drives these diseases. This understanding can affect how physicians determine a patient’s risk of relapse, as well as identify potential treatment strategies and inform new clinical trials.
For example, atypical teratoid rhabdoid tumor (ATRT) is a rare brain tumor that predominantly occurs in young children. Using data gathered through clinical trials, researchers led by Santosh Upadhyaya, MD, were able to study the molecular groups of ATRT and correlate them with clinical outcomes. Published in Clinical Cancer Research in 2021, the findings provided more details about how the three molecular groups of ATRT—ATRT-MYC, ATRT-SHH and ATRT-TYR—behave clinically. The study showed that ATRT-TYR is less likely to metastasize than the other molecular groups, and that ATRT-SHH has the highest chance of metastasis at presentation. While the child’s age at diagnosis and extent of metastatic spread remain the most important factors to consider for prognosis and treatment, the findings will aid the development of new clinical trials.
“If you look at the biology of ATRT, we have learned in the last few years that this is not a single disease but instead there are at least three biologically different groups of the same disease,” Upadhyaya said.
Research has revealed that medulloblastoma, the most common malignant childhood brain tumor, is not a single disease, but that there are actually four molecular groups with different dependencies and outcomes. A 2012 study by Paul Northcott, PhD, Developmental Neurobiology, was key to understanding the medulloblastoma molecular groups. These groups are WNT and SHH (which are driven by their namesake genetic mutations), Group 3 and Group 4. Prognosis for medulloblastoma is different for each molecular group. WNT tumors respond the best, with 95% five-year survival. SHH and Group 4 tumors have approximately 75% five-year survival, and Group 3 has 60%.
Northcott’s research continues to reveal more about medulloblastoma based on molecular diagnostics. For example, a recent study of relapsed disease in the Journal of Clinical Oncology found that 10% of tumors classified as relapsed medulloblastoma are actually secondary malignancies, often high-grade gliomas. Newly diagnosed high-grade glioma and relapsed medulloblastoma may be treated differently so this type of understanding is extremely valuable for clinicians.
“Molecular analysis needs to be included in the diagnosis and treatment of childhood brain tumors,” Northcott said. “Research like ours can provide important context that is clinically relevant for patients.”
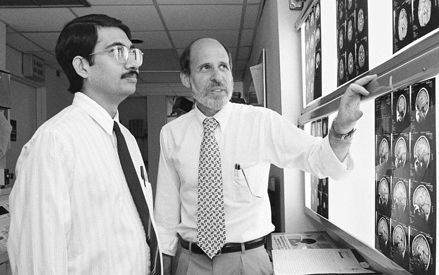
Amar Gajjar, MD, and the late Larry Kun, MD, (L to R) pictured here in 1995, were integral to building the St. Jude brain tumor program to what it is today.
Collaboration underlies progress
When the brain tumor program was established in 1985 by the late Larry Kun, MD, it was among the first to unite neurosurgeons, radiologists, pathologists, psychologists and nurses on one interdisciplinary team. With establishment of the brain tumor program, St. Jude partnered with Le Bonheur Children’s Hospital to fulfill the neurosurgery component of treatment, forming one of the Mid-South’s most successful medical collaborations.
The program has become one of the largest in the world but remains grounded in the idea of collaboration and partnership. Scientists and clinicians will continue to work together to make progress against these diseases, bringing forward creative new approaches for clinical testing.
“When I joined St. Jude, I looked forward to becoming part of a team of dedicated, bright individuals who were committed to expanding the horizons of treatment and research," said Kun upon his retirement from St. Jude in 2016. “Teamwork and collaboration were as important then as they are today when technological and scientific advancements have significantly changed the way that we find cures and save children.”






