St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Environment helps fuel hepatoblastoma in premature infants
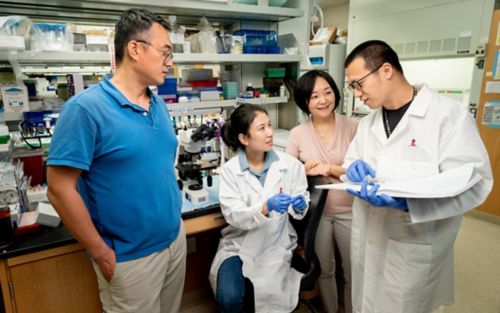
Hepatoblastoma occurs predominantly in very young children and tends to more aggressive when developing in premature infants. Findings from Jiyang Yu, PhD, Li Fan, PhD, Liqin Zhu, PhD, and Qingfei Pan, PhD, reveal why this occurs.
For a seed to sprout, it needs to establish itself in an environment that will promote its growth – with soil, water and sunlight. Cancer is like a seed, which is more likely to grow and spread in a hospitable environment. Findings from St. Jude Children’s Research Hospital have shown that hepatoblastoma, the most common pediatric liver cancer, finds such a hospitable environment in babies born prematurely.
Hepatoblastoma occurs in the liver, the body’s largest internal organ, usually in infants and children under the age of three. It is a rare solid tumor, diagnosed in only around 200 children per year in the United States. Often hepatoblastoma can be treated successfully with surgery after chemotherapy. However, hepatoblastoma becomes more difficult to treat when it grows to involve the entire organ or spreads beyond the liver. More than 60% of children with such high-risk hepatoblastoma do not survive past five years.
Liqin Zhu, PhD, St. Jude Department of Pharmacy and Pharmaceutical Sciences is studying how the interaction between the organ and the tumor contributes to the development of liver cancer. Understanding the interaction will help physicians predict a patient’s prognosis and response to treatment.
The link between prematurity and hepatoblastoma
The incidence of both pediatric and adult liver cancers is increasing worldwide, suggesting that something besides genetics may be at work. Pediatric hepatoblastoma remains rare but the incidence rate is growing at a faster pace than any other pediatric cancer. The suspicion is that the increase is due, in part, to the improved survival of premature infants, since hepatoblastoma is the only cancer whose risk is tightly associated with premature birth.
Premature infants have a 20-50-fold higher risk of developing hepatoblastoma than babies born at full-term. They are also at an increased risk of developing hepatoblastoma that metastasizes. These features strongly suggest that the immature liver provides a favorable tumor environment.
“Pediatric cancers have far fewer mutations than adult cancers, and hepatoblastoma is a good example of this because it is one of the simplest cancers genetically,” Zhu said. “But studies have shown that the genetic alterations found in hepatoblastoma patient tumors, when replicated in research models, only drive this cancer in immature livers, not in adult livers. This suggests that there may be something about the immature organ environment that plays a role in the cancer’s development.”
Zhu and her colleagues reported in Hepatology that hepatoblastoma cells are drastically more metastatic in immature livers than in livers that are more developed. Immature livers also experienced greater levels of hypoxia; a phenomenon caused by low oxygen in the tissue.
Research reveals the mechanism
To understand more about what mechanisms might underlie this phenomenon Zhu and her team collaborated with co-corresponding author of the paper Jiyang Yu, PhD, St. Jude Department of Computational Biology on a single-cell analysis.
“Single-cell sequencing is extremely powerful and a perfect tool to apply here to solve the puzzle of cellular heterogeneity in the complex tumor microenvironment,” Yu said. “My lab has developed computational tools to reveal the networks with and between cells as well as the underlying hidden drivers of cancer. These tools have enabled us to understand how the microenvironment and underlying ligand molecules drive hepatoblastoma metastasis.”
The team found a key signaling pathway that helps promote hepatoblastoma metastasis under hypoxic conditions. This pathway, Cxcl1/Cxcr2, works by the liver secreting the chemokine Cxcl1, which sends signals to its receptor Cxcr2 on hepatoblastoma cells. Chemokines are small signaling protein secreted by cells and are one of the major mediators of tissue inflammation. The researchers found that this Cxcl1/Cxcr2 pathway is only active in immature livers but not in more developed livers. Their work showed that the pathway protects hepatoblastoma cells and fuels their spreading under hypoxia. Together, the findings signal a relationship between the chemokine pathway, hypoxia and metastatic hepatoblastoma.
“This finding is clinically relevant because intermittent hypoxia occurs very often in premature babies whose lung function is not yet well developed,” Zhu said. “While there are studies on the effect of neonatal intermittent hypoxia on the nervous system and the respiratory system since those systems are the most impacted, less was known about hypoxia and the infant liver.”
The activity of the Cxcl1/Cxcr2 chemokine axis may be further enhanced by intermittent hypoxia in premature infants, which will be a future avenue of research.
“Even for adult cancers, targeting just tumor cells is unlikely to be completely successful because some tumor cells may evade treatment as well as drug toxicity,” Zhu said. “But, if you can control the disease promoting conditions in the organ, in the environment, to help quiet down these ‘accomplices’ and combine that with tumor-oriented therapies, that may make a significant difference in patient outcomes.”
“This is important information for the pediatric cancer community,” Zhu added. “We’ve provided a scientific rationale for the importance of controlling chemokine activities in the liver for children with high-risk hepatoblastoma, which may help guide the development of future therapeutics.”






