St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Getting to the bottom of a medulloblastoma mystery
Posterior fossa syndrome occurs in up to 40% of medulloblastoma patients treated with surgery, but what is it really, and how can it be avoided? Researchers at St. Jude now have the answers.
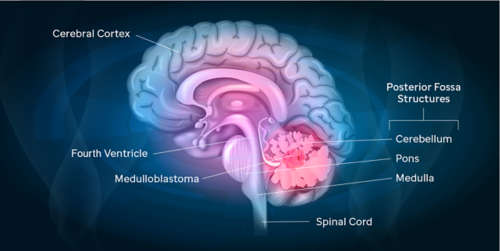
Surgery is a necessary, life-saving treatment for many people with cancer including children who have brain tumors. But an invasive procedure on such a sensitive part of the body as the developing brain can have unintended side effects. This is the case with a condition called posterior fossa syndrome. This syndrome develops in 25-40% of children with the brain tumor medulloblastoma following surgery.
Posterior fossa syndrome occurs with medulloblastoma tumors that arise from the midline section of the lower part of the brain, which separates left and right cerebellar hemispheres. Also known as cerebellar mutism syndrome, this condition is best known for mutism since the affected child often loses the ability to talk after surgery. However, in all cases the mutism subsides, which can lead some providers to downplay this condition as temporary or completely recoverable.
But, posterior fossa syndrome is more complex than has been appreciated. From studying patients at St. Jude who are being treated on the latest medulloblastoma protocol, researchers have better characterized the syndrome and its symptoms. They determined that, in addition to difficulties communicating, the syndrome can cause difficulty walking, involuntary eye and other movements, and behavioral issues and irritability that persist, in some cases, for years. The team’s findings were published recently in the journal Neuro-Oncology.
“There is so much more going on than just the mutism, and it’s occurring in a significant number of patients,” says Raja Khan, MD, St. Jude Neurology. “It is frustrating to see such severely affected children because it not only disables the child but it also can affect their ability tolerate the cancer treatment that they need for cure of medulloblastoma.”
The team was able to classify patients into two groups based on the severity of their symptoms:
- Posterior fossa syndrome type 1: Completely mute, with very restricted movement that includes inability to walk, neurologic deficits, abnormal eye movement and other involuntary movement.
- Posterior fossa syndrome type 2: Limited verbalization, and similar but less severe other symptoms than children with type 1.
Researchers also observed noteworthy cases where children did not have impairment of their ability to talk, but experienced other symptoms of posterior fossa syndrome.
With a new understanding of this mysterious syndrome, and the devastating effect it can have on some patients, the researchers wanted to better understand what causes it and how it might be avoided. Their work highlights a simple shift that could make a significant difference in the lives of children with medulloblastoma.
A focus on surgical expertise
The researchers conducted an analysis of the centers where patients received the surgery needed to treat their medulloblastoma. The scientists were able to distinguish between high-volume and low-volume centers. High-volume surgical centers treated a large number of pediatric brain tumor patients and had a fellowship or speciality for pediatric neurosurgery. Low-volume centers were those for whom a pediatric brain tumor patient was a bit more unusual, and wasn’t one of the conditions most often treated.
The results showed that children treated at high-volume centers by experienced pediatric neurosurgeons had a lower incidence of posterior fossa syndrome. For families and referring physicians navigating the early days of treatment for a child with medulloblastoma, it is important to seek out highly experienced, specialized care from surgeons who often treat this specific type of brain tumor in children.
“We are doing so much in the clinic to try to improve outcomes for patients, from limiting radiation exposures to lowering doses of chemotherapy and trying to preserve hearing, but we’re not making a big push to reduce the cases of posterior fossa syndrome,” says Giles Robinson, MD, St. Jude Oncology. “This study has shown that seeking out an experienced pediatric neurosurgeon can make a dramatic difference for patients.”
The researchers highlight that a family has more agency than they realize to choose the surgeon who operates on their child. Emergency room physicians, and even surgeons themselves should also not hesitate to seek out experienced pediatric neurosurgeons for their patients with medulloblastoma. It could have a profound effect on a patient’s care and quality of life.






