St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
The current landscape and promising future of sickle cell disease therapy
Pain crises are the hallmark symptom of sickle cell disease. But recent advancements in sickle cell disease therapy have clinicians looking to preserve organ function and patient health for potential cures.
Major advancements in the treatment of sickle cell disease have occurred in the last decade. Since a 2011 study recommended hydroxyurea treatment for young children with sickle cell anemia (BABYHUG), three more therapeutic medications have been approved by the FDA as treatments for this catastrophic disease.
In addition, improvements in stem cell transplant options offer a cure for this disease, and significant advances in gene therapy promise additional curative opportunities. However, challenges continue to exist with these curative options, such as access and reduction of toxicities. Let’s take a look at where we are with sickle cell disease therapy.
Sickle cell disease’s diabolical one-two
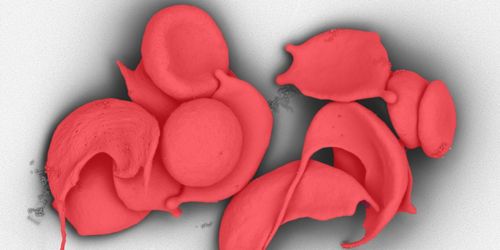
Pain crises are the hallmark symptom of sickle cell disease. They are caused by the sickle-shaped blood cells clogging arteries, limiting blood flow and depriving tissue of oxygen. This causes intense and debilitating pain that can last a few hours or weeks. These sickled cells also clog arteries that deliver blood to organs, frequently resulting in organ damage that causes additional long-term problems.
Teenagers and young adults with sickle cell disease often develop the initial signs of organ damage of the kidney, bone, heart, lung and brain. Unfortunately, organ damage frequently progresses as individuals with sickle cell disease get older, and both the onset, accumulation and progression of organ damage is directly linked to an early death.
Therapeutic landscape for sickle cell disease
Hydroxyurea was a breakthrough in reducing the frequency of pain crises. But the early initiation of the drug likely also delays and, in some cases, prevents organ damage. It inhibits blood sickling by increasing fetal hemoglobin in red blood cells and reduces white blood cells to limit inflammation.
New therapies from the last few years address the sickled cells in other ways. The drugs, including glutamine, crizanlizumab and voxelotor, are also proving to be beneficial. Voxelotor improves anemia and glutamine and crizanlizumab reduce the frequency of pain events. And it appears that these benefits are additive to the benefits of hydroxyurea therapy if a patient is treated with combination therapy.
L-glutamine is absorbed by the sickled blood cells, releasing antioxidants to lower the stress level of the blood cells. Crizanlizumab binds to a molecule on blood platelets and to another on the inside walls of blood vessels. The molecule P-selectin is a known driver of the sickling process, and crizanlizumab blocks the cellular interactions that cause P-selectin to work. Voxelotor helps hemoglobin retain more oxygen and enables the blood cells to retain their normal shape instead of sickling.
But the holy grail of sickle cell disease treatment is preventing organ damage before it starts.
Each patient’s symptoms and severity differ —there isn’t one way to treat every patient. This is one of the biggest challenges to effectively treat and manage sickle cell disease.
Historically, the effectiveness of therapies was gauged by reducing pain events, because they occur frequently and can be measured. But organ preservation is different — it’s difficult to assess it in a clinical trial because it happens over years to decades and few individuals will have damage to any single organ.
Combination therapy and the end goal
While hydroxyurea is important in reducing pain episodes and mortality, it isn’t sufficient by itself. Individuals with sickle cell disease who are treated with hydroxyurea continue to suffer from complications, including some developing organ damage. Fortunately, recently approved therapies show additional benefits to hydroxyurea and have no overlapping side effects. Now we are investigating combination therapies. The goal is to better identify the most effective combination therapy for each patient aimed at reducing pain but, more importantly, also protecting organ function.
Curative therapy for sickle cell disease
In March, St. Jude will host a virtual symposium on stem cell transplantation and gene therapy for sickle cell disease. The event will focus on understanding new technologies related to research, collaborations and the importance of including patients in this process.
I hope that before I retire, I’ll be able to cure pediatric sickle cell disease patients. But we still have a long way to go. In the meantime, we know that the healthier patients who receive curative treatment have better outcomes. Our aim is to use a toolbox approach to multimodal therapy and keep the pediatric population as healthy as possible. Then, when curative therapies are available, they’ll be better candidates, have better outcomes, and ultimately have better quality and quantity of life following their cure.






