St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Immune markers offer clues to antibody production in response to flu
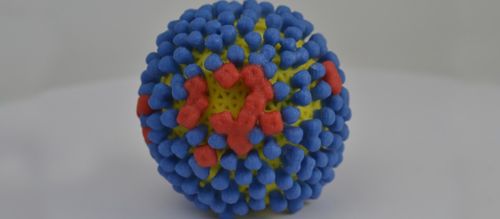
Antibodies provide potent protection against the flu and other viruses. Vaccines are designed to stimulate antibody production. Researchers measure antibodies to gauge the strength of the immune response to the infection.
But questions remain about immune factors that drive the magnitude of the antibody response, including why flu infections do not always trigger a rise in blood antibodies. Better understanding of the multistep process could improve flu diagnosis, vaccine design and strategies to track viral spread.
A study led by St. Jude Children’s Research Hospital scientists identified key immune cells associated with antibody production in response to flu and other viral infections. The findings include the strongest evidence yet in humans that white blood cells called helper T cells (CD4+ cells) are associated with a strong and long-lasting antibody response to flu.
Antibodies also develop in tissue lining the airways. In that tissue, the researchers found that the white blood cells correlated with antibody production were monocytes, not helper T cells.
“The immune factors that explain why some people mount a strong antibody response and others don’t has not been well understood,” said Richard Webby, PhD, of the Infectious Diseases Department. “This study identifies some of those factors, providing information needed to design more effective vaccines for flu and other viruses.”
“Airway monocytes often show up as correlates of severe disease, so it was interesting here to see them also associated with protective immune responses,” said Paul Thomas, PhD, of the Immunology Department. “It points to the fact that many immune factors play protective and pathogenic roles at the same time.”
The findings stem from an analysis of blood collected from patients with laboratory-confirmed flu enrolled in the Southern Hemisphere Influenza and Vaccine Effectiveness, Research and Surveillance (SHIVERS) study. The study was based in Auckland, New Zealand. Researchers also studied immune markers in flu patients enrolled in the FLU09 study conducted in Memphis.
The study appeared in the journal Cell Reports Medicine. Webby and Thomas were the co-corresponding authors.






