St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
COVID-19 vaccine FAQ: Infectious disease and virus experts weigh in
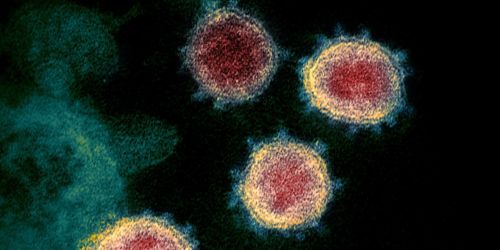
This transmission electron microscope image from NIAID shows SARS-CoV-2, the virus that causes COVID-19. Particles are shown emerging from the surface of cells cultured in the lab. The crown-like spikes on the outer edge of the virus particles give coronaviruses their name. Vaccines being used attack the spikes on the surface.
I recently participated in an online forum on COVID-19 vaccines with Richard Webby, PhD, answering and commenting on common questions about the vaccines. I am a St. Jude faculty member and physician in the Infectious Diseases department. Webby is a researcher in the Infectious Diseases department and director of the World Health Organization Collaborating Center for Studies on the Ecology of Influenza in Animals and Birds. Here are some of the questions we answered.
Question: Can you describe the vaccine status? What are they targeting in the virus and do the vaccines work?

Richard Webby, PhD
Webby: In the U.S., there are two COVID vaccines in use, but there are many, many more in the development pipeline. These vaccine platforms are of all shapes and colors and flavors — it's really been a kitchen sink approach. A common theme of many of these vaccines is that they primarily target one virus protein — they have one active ingredient, if you like. They target the spike protein on the surface of this virus.
Preclinical studies of vaccines that targeted the spike protein showed that this approach could completely clear the virus from lungs of vaccinated animals. Based on those results, going forward with a vaccine was clearly the way to go.
Q: How many COVID vaccines doses do we expect and how do they perform in comparison to the flu vaccine?
Webby: In the US, we’re up to 300 million ordered doses of the Pfizer and Moderna vaccines, which are the ones currently in use. With the Johnson & Johnson vaccine already under U.S. Food and Drug Administration review, you have a potentially game-changing, single-dose adenovirus vaccine on its way as well.
At the beginning, the FDA set a target of 50% effectiveness for approval of COVID vaccines. The current vaccines approved and soon-to-be-approved for emergency use authorization have easily met that criteria. Conversely, the annual flu vaccine struggles to achieve 50% effectiveness. In part, that’s because of the nature of the flu virus, which mutates more. Flu vaccines are also less immunogenic and trigger a weaker immune response.
Q: We’ve received the vaccine – are we completely protected?
Webby: The primary endpoint in COVID-19 vaccine trials is protection from severe disease, meaning hospitalization or death. It's easier for a vaccine to get the virus out of the lower respiratory tract, and that’s important as the virus replicating there is what causes more severe disease. But with transmission and infection, we have to worry more about the upper respiratory tract. We currently lack much information on the performance of COVID vaccines in protecting the upper respiratory tract. Can these vaccines protect us from getting infected, carrying it, or even transmitting it to others? The short answer is we don’t know, which is why we keep on bearing this message — Even if you are vaccinated, you still need to wear a mask and keep your physical distance. We just don’t have enough information yet.
Q: How are COVID variants changing things? Do the vaccines protect against the COVID mutations?
Webby: We anticipated the virus would mutate as it spread, and that’s exactly what it’s doing. The three variants of concern in the news right now are more transmissible or appear to be more transmissible. The B.1.1.7 variant that emerged in the U.K. appears to be pretty similar antigenically to what's in the vaccine. The P.1 variant that emerged in Brazil and the B.135 variant that emerged in South Africa actually look to be a little bit different. The B.1.1.7 variant is everywhere, including the U.S. The B.135 and P.1 variant have been seen in a few countries but isn’t as widespread as B.1.1.7. Over time, we’ll likely see community spread of these variants and also identify more variants. While data are still accumulating, the good news is that current vaccine effectiveness, where it has been measured, still appear to meet the FDA criteria for approval, even against these variants.
Q: Do COVID-19 vaccines cause infertility problems?
Hijano: There is really no evidence that the vaccine can cause infertility. The Yale School of Medicine concluded that the vaccine’s proteins do not interact with the placenta. We also know that women who’ve recovered from COVID-19 don’t have antibodies that react against the placenta. There’s also no evidence of infertility among women who have recovered from COVID-19. Furthermore, women have conceived after coronavirus infection and vaccination.

Diego Hijano, MD
Q: What about pregnancy?
Hijano: Pregnancy is a risk factor, including for severe COVID-19 complications. If you are pregnant and you have COVID-19, you are more likely to be hospitalized and to need intensive care and mechanical ventilation. COVID-19 can also affect the fetus by increasing the risk of preterm delivery. The vaccines do not enter the nucleus of the cells and will not enter human DNA, so they cannot cause any genetic changes to the fetus. Vaccines also do not appear in breast milk. That is because the vaccines are made of fats that won’t enter a mother’s bloodstream and get to the breast tissue. The general consensus is that for women who are pregnant, nursing or trying to conceive, contracting COVID-19 is almost certainly more dangerous than getting immunized. Women in these categories should consider being immunized.
Q: Who should be concerned about receiving a vaccine?
Hijano: People who had a severe allergic reaction (e.g., anaphylaxis) or immediate allergic reaction after a previous dose of an mRNA COVID-19 vaccine or any of its components (including polyethylene glycol ) should not receive the vaccine. In addition, people with history of allergic reaction to polysorbate (due to potential cross-reactive hypersensitivity with the vaccine ingredient PEG) should not receive the vaccine. Other allergies to pets, foods or medicines like penicillin or sulfa drugs, are not a contraindication to the COVID-19 vaccines.
Q: Should individuals with a history of COVID-19 be vaccinated?
Hijano: Cases of reinfection show us we cannot rely on immunity acquired by natural infection to confer herd immunity; this strategy is dangerous and ineffective. Herd immunity requires safe and effective vaccines and robust vaccination programs. Vaccination of people with active SARS-CoV-2 infections should be deferred until the person has recovered from the acute illness (if the person had symptoms) and have met the criteria to discontinue isolation. This recommendation applies to people who experience SARS-CoV-2 infection before receiving any vaccine doses as well as those infected after the first dose but prior to the second dose.






