St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Tumor microenvironment switches from homely to hostile when this process is turned off
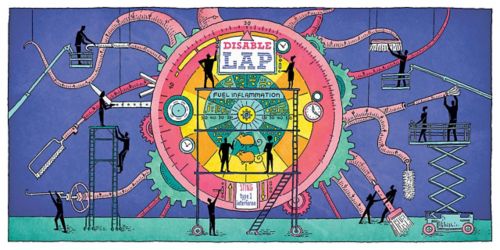
LAP is the cellular process that turns cell macrophages into tumor cell housecleaners. Research suggests disabling LAP turns those macrophages into tumor cell killers.
Most cancer research involving immunotherapy and anti-tumor immunity focuses on reversing T-cell suppression, meaning, the cancer cells actively thwart the body’s efforts to kill the cells.
My lab took a different approach, and we were knocked out by the results.
What is the tumor microenvironment?
This is the cellular environment where the tumor exists. In this ecosystem, the tumor cell engages in regular activity and influences what happens around it. And, as with any other cell, myriad interchanges are taking place. Disrupting that environment can provide opportunities to attack the tumor cell. We found one such interchange more than a decade ago.
LAP and the tumor cell
We discovered LC3-associated phagocytosis in 2007. Known as LAP, it is a normal cellular process that helps degrade dead and dying cells. This waste material is then disposed by macrophages, white blood cells that are part of our immune system. Macrophages essentially eat the cellular debris. They also attack tumors. So, the question is, how do we get macrophages to attack the tumor instead of “cleaning up” the tumor microenvironment?
Here’s where it gets complicated: We needed to first distinguish between macrophages prompted by LAP and another cellular degrading process known as autophagy, where a cell shuts itself off. The reason behind this is that many of the same proteins and signals are involved in each process.
LAP is the key to fighting tumors
Here’s what we did – Narrowing down the genes involved in LAP and not autophagy revealed that LAP indeed was the process behind the macrophages’ behavior. Without LAP, molecules to signal the anti-tumor response, like STING and type 1 interferon, increased — meaning, LAP was the process that dialed those molecules back. In other words, targeting LAP could promote an anti-tumor response and slow tumor growth.
We still need LAP
Cells still need to be able to function. Dead cells still need to be taken care of. We’d previously found in preclinical models that defects in LAP can lead to autoimmune disorders. Ideally, we’d like to suppress the LAP process for tumor fighting, and then reintroduce the process so the body can resume normal cellular functioning. The cool part this research reveals is that we may have a means to treat some tumors simply by reassigning the cells designed to carry out the tumor cell’s housecleaning process. Finding compounds and processes that would allow us to regulate LAP is the next step.






