St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Pediatric melanoma mystery solved by genome sequencing research
Because of the information provided through whole-genome, whole-exome and whole-transcriptome sequencing, researchers were able to identify an important genetic mutation in melanoma.
Sophie Spitz, MD, published the first cases of melanocytic skin lesions in children in the late 1940s — these lesions became known as benign Spitz nevi and their cancerous counterparts, spitzoid melanoma. Spitzoid melanoma is the most common skin cancer of childhood and adolescence and — although technically a melanoma — is very different from aggressive melanomas commonly seen in adults.
Most people have never heard of Dr. Spitz, nor do they realize that kids can develop melanoma. Before I came to St. Jude, I was one of them, but one brave child changed that. I’ve never met him, I don’t know his name, but I do know his genome better than anybody else in the world. My team and I uncovered the genetic changes that drove his tumor, and this single patient may help change outcomes for future melanoma patients regardless of their age.
The challenge
I joined St. Jude because of the Genomes for Kids (G4K) clinical trial. Back in 2015, when it launched, barely anybody was sequencing whole genomes, exomes or transcriptomes from large numbers of cancer patients and certainly nobody was offering this as a clinical test. G4K focused on moving next-generation sequencing into the clinic and, as I wanted to work on the cutting edge, I moved to Memphis from Atlanta. Among the questions we hoped to answer was the clinical utility of whole-genome, whole-exome and whole-transcriptome sequencing – can the genetic patterns of a tumor help us get a better diagnosis, understand how aggressive the disease might be or uncover a new therapeutic option.
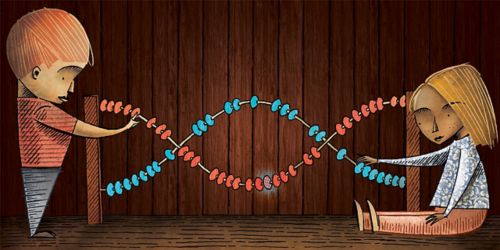
Whole-genome sequencing involves determining the order of the 3 billion letters (chemical bases) encoded in the cell’s DNA. The exome includes just the 1-2% of the genome that encodes instructions for assembling proteins. The transcriptome identifies genes being expressed. By using these three approaches together, we hoped to get a comprehensive view of every single genetic change in a patient’s tumor, but interpreting all of that data is a daunting task.
My team are clinical genome analysts: a hybrid between PhD cancer biologists and computer programmers, and our job is to hunt through vast amounts of genome sequencing data for rare pieces of information that can benefit the patients. Sequencing data generated from tumors and matching normal blood or skin by our colleagues in the clinical sequencing lab is run through a sophisticated data analysis pipeline developed over the last decade by my boss, Jinghui Zhang, PhD, and many other members of the Computational Biology department. The analysts sit at the end of the process, checking and curating the changes that the software pipeline predicts. We look for the genetic alterations (mutations) that can help us better understand the child’s disease. What genetic mutations drove the tumor? How did it evolve over time and treatment and what are its vulnerabilities? It is not unusual for an analyst to spend days on a complicated case, mining the medical literature and running additional computational analyses to get an answer.
Pathway to tumors
The first spitzoid melanoma genome that I ever analyzed was from the patient I mentioned earlier. Melanoma in adults typically includes RAS/MAP kinase pathway mutations that play a role in tumor initiation. Kinases are enzymes that function as “on/off” switches to regulate gene activity. We know much less about the genetic drivers of spitzoid melanoma in kids. At the time, we had no idea what genetic changes drove around half of them — perhaps some unknown kinase was responsible?
My analysis revealed plenty of mutations in the tumor, including a deletion of CDKN2A/B and an alteration of the TERT gene – both known to play a role spitzoid melanoma. But the tumor carried none of the famous kinase mutations associated with either adult melanoma or spitzoid melanoma in kids. This didn’t make any sense. There should be a kinase driver, and I was going find it.
As a genome analyst, I hate attending the weekly tumor case review meetings with nothing to offer. So, I looked down the long list of other gene alterations and way down at the bottom was a rearrangement in a gene called MAP3K8. The “K” in MAP3K8 means “kinase.” In fact, the “3K” in MAP3K8 means “kinase, kinase, kinase.” I was on to something. I spend the rest of the day digging through scientific papers on kinases and by the time I left, I was convinced that MAP3K8 was the kinase driver of this tumor.
The MAPK-MEK relationship in tumors
BRAF is, perhaps, the most famous cancer gene. BRAF is a kinase and part of the RAS/MAP kinase pathway; mutations in this gene drive adult melanoma as well as many other cancers. BRAF switches on a protein called MEK and MEK in turn switches on a whole set of other proteins involved in cell growth and division. Mutant forms of BRAF are hyperactive, so it is easy to understand why melanomas with such mutations grow uncontrollably. A few years ago, small molecule inhibitors of mutant BRAF were approved for treatment of melanoma. The study that I had found, from a group at Harvard in 2010, showed that tumors expressing high levels of a certain gene are resistant to BRAF inhibitors. That gene was MAP3K8 and the study went on to show that MAP3K8 can switch on MEK – just like BRAF. Based on three other studies that I found, it was clear that the MAP3K8 mutation that in the patient’s tumor hyperactivated the protein and that, perhaps, this was spitzoid melanoma’s equivalent of BRAF.
We began treating the patient with trametinib, a precision medicine that inhibits MEK, blocking the downstream effects of mutant MAP3K8. Amazingly, the patient’s tumors shrank as he responded to the targeted therapy. Good news for one patient, but how about others with spitzoid melanoma? Was this just a lucky one off or could we find MAP3K8 mutations in other tumors too? I spent most free moments for the next year reading papers and downloading tumor data from other published studies with which to mine using our algorithms. The problem is, there’s virtually no data from spitzoid melanoma in the public domain, and all there was to mine was data from adults. As I had come up with nothing, we decided to write a small case report and try to get it published in a dermatology journal in the case it might be useful for somebody else one day.
About a year later, one of the analysis team came to my office and asked for my opinion on a case. Tonya is our brain tumor specialist, but she was analyzing the solid tumors that week since I had been out attending a conference. She had found “an interesting kinase mutation in a melanoma” and went on to mention “a paper from 2010” suggesting a mode of action involving MEK. I immediately called the pathologist who had ordered the testing, Armita Bahrami, MD. We had worked on the first tumor together and she knew all about MAP3K8. “Armita,” I said, “we’ve found another one.”
Over the next year, Armita got us permission to study spitzoid tumors from 49 other patients, Jinghui’s lab ran the genome sequencing and pushed the data through the computational pipeline, and Tonya and I analyzed the results. To our amazement, we found that 33% of the patients carried similar MAP3K8 mutations. In fact, MAP3K8 is the most commonly mutated gene in pediatric spitzoid melanoma. Now that I knew exactly what I was looking for, I went back to the adult melanoma data armed with a new program that my colleague Steve (a computer scientist who I used to share an office with) wrote. Steve’s program zipped through 472 adult melanoma transcriptomes in less than a minute and found seven (1.5%) with MAP3K8 mutations.
Nearly 100,000 cases of melanoma are diagnosed in the U.S. each year, including about 1,000 to 2,000 children. The fact that MAP3K8 switches on MEK and that the first patient responded to a MEK inhibitor points to a new therapy option for tumors with MAP3K8 mutations in either children or adults.
We found this important genetic mutation is because we were doing the hard experiment — we sequenced the whole-genome, whole-exome and whole-transcriptome because we needed the complete genomic picture. If we’d been doing anything less, we would have missed it.






