St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Life after cancer: Researchers work to understand and ease the cognitive challenges that childhood cancer survivors face

Kevin Krull, PhD, a member of the St. Jude Department of Epidemiology and Cancer Control, has shaped our understanding of the cognitive problems that cancer survivors face. His work focuses on developing strategies to address, reduce or prevent the cognitive effects of cancer therapy.
Childhood cancer, particularly pediatric acute lymphoblastic leukemia, is one of the great medical treatment success stories of recent decades. But survivorship often comes at a price. Research from St. Jude has helped broaden and deepen our knowledge of the challenges faced when survivorship begins in childhood or adolescence.
Kevin Krull, PhD, a member of the St. Jude Department of Epidemiology and Cancer Control, has helped redefine our understanding of the cognitive problems that survivors face, particularly identifying who is at risk and why. He is also working to develop more effective strategies to address, reduce or even prevent cognitive effects.
Krull’s interest in neurotoxicity and the body-mind connection began early in life.
“I grew up in Detroit. By junior high school I had seen the effects of alcohol and drug use and other toxins on how people function and behave,” he said. “During my training I became particularly interested in the developing brain.”
He earned a doctorate in clinical psychology and neuroscience. While Krull was finishing a postdoctoral fellowship, Leslie Robison, PhD, was organizing the landmark Childhood Cancer Survivor Study (CCSS). Funded in part by the National Cancer Institute, the study uses periodic surveys to track health and other outcomes for almost 20,000 childhood cancer survivors and their siblings who were not pediatric cancer patients.
The study is now headquartered at St. Jude where Robison chairs the Department of Epidemiology and Cancer Control. CCSS laid the foundation for mapping the late effects of pediatric cancer treatment and fueled efforts to minimize or prevent their influence.
Krull joined St. Jude in 2007, the same year the St. Jude Lifetime Cohort study (St. Jude LIFE) opened. St. Jude LIFE participants are long-term St. Jude childhood cancer survivors who return to the campus for several days of tests to measure their health and well-being. Today, more than 3,500 St. Jude cancer survivors have joined the study and undergone comprehensive health assessments. Both CCSS and St. Jude LIFE aim to improve life for childhood cancer survivors now and in the future.
At this year’s annual meeting of the American Society of Clinical Oncology in Chicago, Krull will provide an update on the unique cognitive needs of pediatric, adolescent and young adult cancer survivors. He will also discuss research into ways to ease or even prevent cancer-related cognitive complications. The June 5 educational session is titled “Managing Cognitive Changes in Cancer Survivors.”
He recently took time to answer some questions on the topic.
St. Jude Progress: What are common cognitive challenges that pediatric, adolescent and young adult cancer survivors face?
Kevin Krull: As more children and young people survive their cancer and we follow them for decades, not just years, it has become apparent that cognitive late effects are more widespread among survivors than previously recognized and that multiple factors are involved. Patients’ age at diagnosis, their sex, genetic makeup, the diagnosis itself and treatment can all play a role.
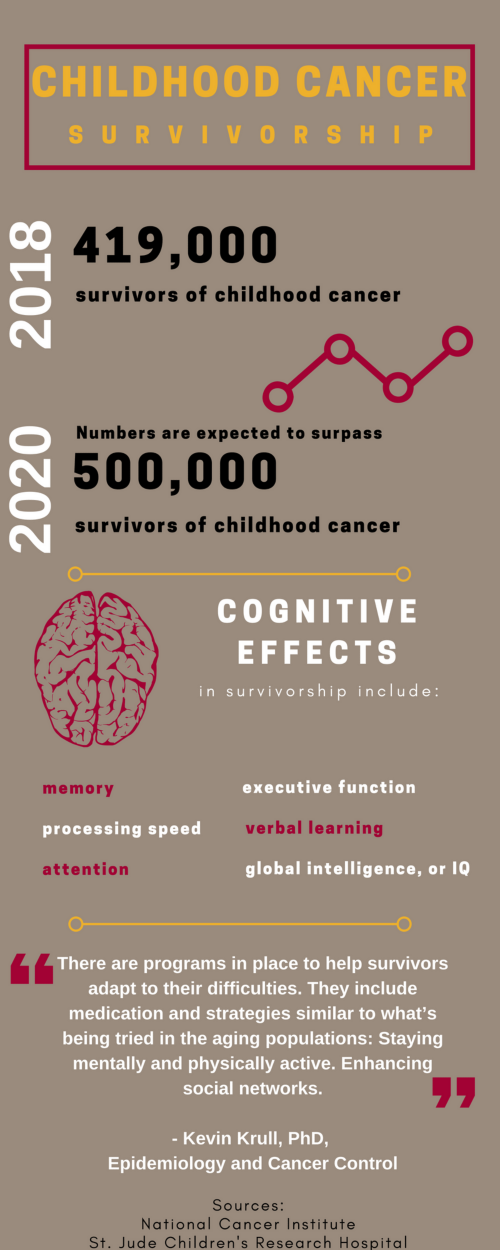
We now know that adult survivors of cancer in childhood or adolescence are more likely than their siblings or those without a diagnosis of pediatric cancer to develop cognitive problems related to memory, attention, processing speed, executive functioning, verbal learning and, in some cases, global intelligence, or IQ.
These deficits can have a life-long impact on survivors, affecting their educational achievement and employment, even decades after their cancer treatment ended. The cognitive issues help explain why, as a group, childhood cancer survivors are less likely to graduate from college, marry or live independently. They are also more likely to report depression and anxiety.
SJP: What are some of the other factors that influence survivors’ risk of cognitive problems?
Krull: Adult cancers typically occur after individuals have completed their education and built a life for themselves, personally and professionally. They may have a spouse or partner and a support network of friends and relations. They have had an opportunity to build a cognitive reserve and have developed skills that almost become automatic. This cognitive reserve provides a cushion if a brain injury occurs. There is extensive literature that shows adults respond to brain injury based on their cognitive reserve. People with good cognitive reserve may lose some skills following a brain injury, but many still function independently in society.
In contrast, cancer in children and adolescents occurs before the brain is fully developed. The disease and its treatment may even limit brain development and affect how far survivors get educationally, behaviorally and socially, and this can limit their ability to build a good cognitive reserve. As some survivors of pediatric cancer age, their primary support is their family. Since they are less likely to develop strong social relationships, they may become overly dependent upon their parents, which cannot last for the life of the survivor.
Unlike survivors of adult cancers, young children and adolescent survivors of cancer often have years or decades of life ahead. In terms of their brain function, there is a bigger window in which toxicity can build and have an impact over time.
SJP: How has understanding of the cognitive challenges facing pediatric cancer survivors evolved during your career?
Krull: With longer follow-up and information gleaned from survivors themselves through CCSS and St. Jude LIFE, we know that cognitive problems are not limited to survivors of brain tumors or those who received neurotoxic therapies such as cranial irradiation or intrathecal methotrexate. We recently published research in JAMA Oncology showing that leukemia itself, not just side effects related to its treatment, may increase the risk for long-term problems with attention, organization and related neurocognitive skills in survivors of acute lymphoblastic leukemia.
In addition, we used to think that cognitive deficits were only late effects that would surface three, four or five years after a cancer diagnosis. We now know that problems surface within six months of diagnosis. These are not just changes seen in brain imaging and markers, but declines in processing speed and reaction time. By following patients and survivors routinely, we realized that performance-based changes occur much earlier than was thought. More importantly, we realize that things change over time and that you have different sources of problems that come and go over time.
Patients may develop cognitive problems during the acute phase of treatment due to toxicity and then recover, or get worse or have new problems emerge. Sometimes those cognitive problems are directly associated with neurotoxicity, but sometimes the problems are secondary to other treatments.
For example, we know that injecting methotrexate into the cerebral spinal fluid is directly related to changes in white and gray matter in the brain, and cognitive function in childhood leukemia survivors. But children with leukemia also get anthracyclines, chemotherapy agents that can cause cardiac problems over time. Those cardiac problems could also cause problems cognitively.
SJP: What are some of the implications of this growing realization of how secondary treatment effects can influence cognitive function?
Krull: The exciting thing is that when we understand it may take 10 years for a survivor to develop a cardiac problem because of anthracyclines, and that the cardiac problems will be related to cognitive problems, that gives us 10 years to intervene. Treating the cardiac problems may help survivors avoid cognitive problems. So every time we discover this link, it opens up a new avenue for potential treatments.
It's not just cardiac problems either. Pulmonary, sleep, endocrine … there are all sorts of other secondary complications that affect memory, attention, executive function and other aspects of cognitive functioning. This is partly why we see the cognitive problems not just in leukemia and brain tumor patients, but in survivors of Wilms' tumor, Hodgkin lymphoma, neuroblastoma and others, none of whom received neurotoxic therapies. None of those patients received brain radiation or intrathecal methotrexate. They received other therapies that affect their body and their organ system, kidney, liver, heart, lungs.
So taking a snapshot of a long-term survivor, there may be all sorts of sources for the problems they're having, not necessarily just their original treatment.
SJP: What’s on the horizon for pediatric cancer survivorship?
Krull: There are ways to help survivors now and research is underway exploring strategies to prevent or ease cognitive late effects in the future.
There are programs in place to help survivors adapt to their difficulties. They include medication and strategies similar to what’s being tried in the aging populations: Staying mentally and physically active. Enhancing social networks. Cognitive strategies like lists, charts and organization to compensate for memory problems.
We have training programs to see if we can help improve cognitive skills or healthy behaviors that have a secondary impact on the cognitive skills. There are also programs in place now to test whether we can prevent, pharmaceutically and behaviorally, some of the cognitive deficits survivors may face.
For example, the current St. Jude Total Therapy Study 17 for children and adolescents newly diagnosed with acute lymphoblastic leukemia and lymphoma includes an intervention led by my colleague Lisa Jacola, PhD, that comes online during active therapy. The program is designed to engage and enrich neural networks through practice-focused training of cognitive skills. The goal is to build up cognitive skills before they decline. So while physicians are working to reduce treatment toxicity while maintaining high cure rates, we are trying to build cognitive reserves that may help survivors to remain functional in society despite cognitive declines.
Other interventions are being tried in other St. Jude clinical trials, including SJMB12 for young people with the malignant brain tumor medulloblastoma. They range from antioxidant supplements and exercise to online computer brain training to bolster attention and memory.
There are many other pharmaceutical agents and procedures that can be used, that theoretically would work to help buffer the chemotherapy treatments. What we don't know at this point is whether they interfere with the efficacy of the chemotherapy on the cancer. That's what we want to avoid. Preclinical studies are needed to answer those questions.
SJP: What help is currently available for survivors with cognitive problems?
Krull: We have programs to teach people how to adapt to their cognitive difficulties. These include enhanced self-awareness of events and circumstances when the problems occur, using strategies to compensate for memory problems. We have programs where we can help train some of the cognitive skills and stimulate underlying neural networks to better benefit from this training.
We also have programs where we can help work on some of the healthy behaviors that may be having a secondary impact on the cognitive skills. For example, survivors are at risk for developing sleep difficulties. Later this year, we expect to start an intervention to see if we can improve survivors’ cognitive function by teaching them healthy sleep hygiene. Similar interventions are in the works to see if survivors benefit cognitively from enhanced cardiopulmonary function.
SJP: What can survivors do now to safeguard cognitive functioning?
Krull: There are many steps individuals can take to improve their health, including their cognitive health. Be more physically active. Eat a healthy diet. Get enough sleep. Be an active learner and practice cognitive skills. The brain needs exercise just like the body does; though instead of just physical exercise, mental exercise is important too. Both should become lifelong habits. Use strategies like making lists to manage challenges. These are things we all should be doing, but cancer survivors might be even more sensitive to the effects of such behaviors than the rest of us, so healthy habits might be even more important for them.
Krull will offer additional insight about the unique cognitive needs of pediatric, adolescent and young adult cancer survivors when he speaks at ASCO Tuesday at 8:20 a.m. The educational session is set for room S504 in McCormick Place.






