St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Kids aren’t little adults when it comes to pediatric MDS
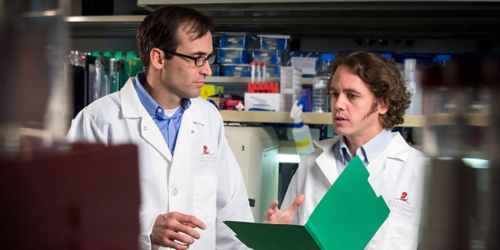
Mutations involved in pediatric myelodysplastic syndromes can result in leukemia. Jeff Klco, MD, PhD, (left) and Jason Schwartz, MD, (right) found MDS is markedly different between adults and children on a molecular level.
On a molecular level, myelodysplastic syndromes (MDS) is very different between adults and children.
MDS, also called myelodysplasia, is a disorder of the bone marrow where blood cells look abnormal, and mature cells are decreased in the peripheral blood, leading to infections, bleeding and anemia. This can occur after chemotherapy, but frequently happens without any known cause. MDS normally occurs in adults around 70, but it also occurs in children. We initially believed the mutations causing MDS in children and adults were different.
Same name, but different driving mechanism
A common mantra in the field of pediatrics is that “children are not simply little adults,” and must be treated and thought about separately. This is certainly true with regard to drug metabolism, physiological responses, and even reactions to some common infections. Our lab’s recent work, published in Nature Communications, shows these differences even reach to the molecular level in some diseases, namely MDS.
Pediatric MDS differs from adults in several ways, including differences in the amount of cells in the bone marrow as well as which chromosomes are lost in bone marrow cells. Using whole exome and RNA sequencing, we now confirmed the genomic landscape of pediatric MDS is substantially different than adult MDS, and our findings may provide new treatment options for children with MDS.
New MDS predisposing gene family
A new class of mutations in the germline of children with MDS finally explains how MDS occurs within families. Our lab found that germline mutations in two genes (SAMD9 and SAMD9L) occur in almost 20 percent of our cases. Curiously, all these children had the same cytogenetic abnormality, monosomy 7, in their bone marrow cells. Both SAMD9 and SAMD9L are located on chromosome 7, and mutations in these genes are tightly associated with chromosome 7 loss. This new knowledge adds to the small number of genes known to predispose children to MDS and will guide treatment and genetic counseling for these patients and their families.
A bad gain leads to a bad loss … and future projects
Our studies and others suggest these mutations prevent cells from growing. Shockingly, the bone marrow cells that can grow frequently eliminate the mutated gene by selectively losing the chromosome (chromosome 7) that contains the mutation. It appears this chromosomal loss, also called aneuploidy, is an adaptive response to these germline mutations, and provides cells a way to circumvent these growth suppressive mutations. Unfortunately, this monosomy 7 can also lead to MDS and even acute myeloid leukemia. To our knowledge, this appears to happen more frequently in childhood, as these mutations can be inherited from parents that lack features of MDS, further confirming that despite sharing a name, pediatric and adult MDS are indeed different diseases.
This is an exciting new model of cancer development, and we are developing new approaches, in particular induced pluripotent stem cells, to better understand this process of adaptive chromosome loss and how it may be triggered.
Jason Schwartz, MD, a Physician-Scientist Training Program fellow in the St. Jude Department of Oncology, contributed to this blog post.






