St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Fat Chance: 'Skinny Gene' research unexpectedly leads to tumor breakthrough
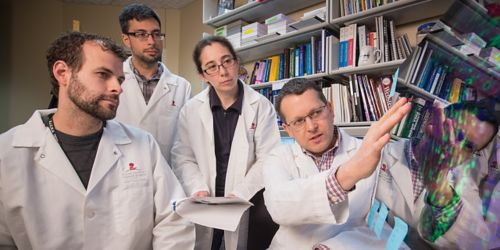
St. Jude Oncology researchers Jason Hanna, PhD, Matt Garcia and Cath Drummond, PhD, look on as Mark Hatley, MD, PhD, explains how endothelial progenitor cells that normally develop to form the lining of blood vessels can also develop into RMS tumors between muscle fibers.
Rhabdomyosarcoma (RMS) is not exclusively a “muscle cancer.” Oncologists and developmental biologists had suspected this for years, but what we didn’t know is where or how it develops. And we would probably still be in the dark if a fellow biologist had not shown me the puzzling tumors appearing in one of his preclinical models—from a project exploring a genetic control for body fat.
That’s right. A wrong turn in the search for the “skinny gene” uncovered an important clue for pediatric RMS tumor research. That clue eventually led to our team’s recent findings, published in Cancer Cell, that pinpointed one of the origins of RMS tumors.
Rhabdomyosarcoma and kids
RMS is the most prevalent soft tissue cancer in children. The survival rate for RMS, when caught early enough, is 70%. That figure hasn’t improved much since the early 1970s, when the current chemotherapy protocol was introduced. And for children who have the highest-risk form of RMS, the survival rate can be as low as 20%. We have to do better, and a better understanding of the machinery of RMS could enable entirely new treatment approaches.
How I got involved
I started looking for answers about RMS as a post-doctoral fellow at the University of Texas Southwestern Medical Center in Eric Olson’s molecular biology lab. Dr. Olson is well known for his genetic research related to muscle, and his pathbreaking work around muscle development and disease is what led to my research into RMS. In fact, he introduced me to Martine Roussel and Charles Sherr, who encouraged me to continue my work in St. Jude Oncology’s Solid Tumor Division in 2011.
Searching for the cheese in the RMS maze
If you look back through decades of medical literature—and even in current search engine results—RMS is described as an arrested state of muscle development that comes from muscle precursors. Yes, the tumor cells look like muscle cells under the microscope and the disease often affects muscles. But not always.
We always wondered about the paradoxes: Rhabdomyosarcoma also occurs in places that don't have skeletal muscle, including the bladder, prostate, salivary glands, gallbladder, liver and abdominal fat. There was never a satisfactory explanation for this. How do the tumors begin?
To start picking apart this problem, I needed to be able to reproduce RMS in the lab. I added cancer-causing RAS proteins and deleted tumor suppressor genes at various stages of muscle development in preclinical models. Tumors formed, but they were never RMS tumors.
Unexpected help from the “skinny gene” researcher
At about the same time, a fellow UT Southwestern scientist, Jonathan Graff, was “successfully” producing RMS in models—unintentionally. He was studying the development of body fat, not cancer. In fact, he was probably as frustrated by producing rhabdomyosarcoma as I was by failing to produce it.
Fortunately, Dr. Graff suspected that his problem might lead me to a solution in my tumor research, and he was right. From there, I worked with a continuing hypothesis that these tumors originate in metabolic “brown fat” cells. But after another six years of experiments, my research team and I discovered that RMS will actually develop in the interior walls of blood vessels—specifically in endothelial progenitor cells.
That could explain how RMS tumors appear in so many locations; every part of the body has blood vessels.
Now that we have figured out where some RMS tumors develop, we want to learn how that transformation happens, to press forward in improving its diagnosis and discovering new treatments. Ideally, we want to pave the way for developing a tumor-inhibitor drug for patients with known predispositions to RMS.
You can read the full article at Hedgehog pathway drives fusion-negative rhabdomyosarcoma initiated from non-myogenic endothelial progenitors. Cancer Cell. January 2018 vol. 33, Issue 1, p108–124.e5.






