St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Cell necroptosis: Can ESCRT-III proteins protect cells from the kill switch?
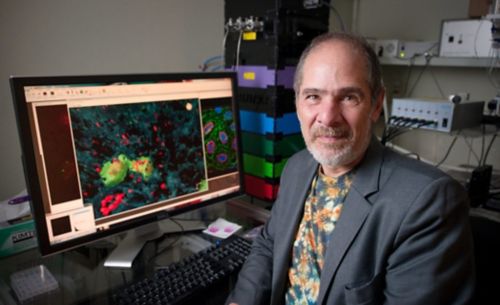
Douglas Green, PhD, and his lab recently discovered a set of proteins that delay or even prevent necroptotic cell death. This has clinical implications for patients fighting infections and possibly thwart the spread of cancers.
It's ironic that maintaining the health of our bodies can often mean killing off our own cells. For example, as the body grows and remodels itself, it needs to get rid of unneeded cells, like knocking down a wall to build an addition to a house. This precisely regulated cell suicide is called apoptosis, and each day your body kills off between 50 billion and 70 billion cells in this way. The average child—whose body is actively "remodeling"—disposes of about 20 billion to 30 billion cells a day through apoptosis.1
The body also operates an aggressive cell suicide program called necroptosis to kill damaged cells or those infected by viruses or bacteria. We scientists have always thought of necroptosis as a pretty inevitable path to destruction for such cells, given that the body needs to get rid of them as quickly as possible.
According to the Chinese legend, in ancient times, a titanic battle between gods destroyed one of the pillars holding up the sky. The pillar’s collapse opened a hole in the heavens, cracking the Earth and causing great devastation—fires, floods and marauding animals. The goddess Nüwa, who had first created humans, took pity on them and using colored stones, patched up the sky, giving it the many hues it has today. She also restored the pillars, controlled the floods, quenched the fires and drove away the wild animals. In many ways, this rescue protein could be described as the biological equivalent of Nüwa.
According to the Chinese legend, in ancient times, a titanic battle between gods destroyed one of the pillars holding up the sky. The pillar’s collapse opened a hole in the heavens, cracking the Earth and causing great devastation—fires, floods and marauding animals. The goddess Nüwa, who had first created humans, took pity on them and using colored stones, patched up the sky, giving it the many hues it has today. She also restored the pillars, controlled the floods, quenched the fires and drove away the wild animals. In many ways, this rescue protein could be described as the biological equivalent of Nüwa.
So it was a real puzzle to us when experiments by us and others found instances when cells would activate the necroptosis "kill switch," called MLKL, but the cells didn't die! Somewhere in the cell was mysterious machinery that gave these cells a stay of execution. While such a delay might seem to be a bad thing, we realized that controlling necroptosis could actually offer a golden opportunity for patients.
For example, during kidney transplantation, the donor kidney suffers necroptosis due to lack of oxygen. If we could control that necroptosis using drugs, we could prevent that damage, resulting in more viable transplanted kidneys.
Delaying necroptosis could also aid in fighting infection. During infections such as influenza, the immune system is alerted to battle the invading virus via chemical alarm signals sent out by infected cells. If we could delay the necroptotic death of those infected cells, they would have more time to send out more alarm signals, to enhance the immune system's ability to battle infection.
We could even thwart the spread of cancers if we could control necroptosis. Tumor cells circulating in the bloodstream seek to spread into body tissues by damaging cells in blood vessel walls, so that necroptosis will kill them, opening a pathway into the body for the cancer cell. If we could thwart that process, we might be able to slow or prevent cancer metastasis.
Also, we know that neurodegenerative disorders such as Lou Gehrig's Disease involve necroptotic death of brain cells. Controlling this suicide process might help preserve those cells.
Fortunately, we had in our laboratory a master scientific sleuth, Yi-Nan Gong, PhD, who set out to trace the machinery that rescues cells from necroptosis. We already knew that MLKL kills cells by piercing the cell membrane to cause the cell to "bleed out" its contents. In studies with cells, Gong and our colleagues at St. Jude and elsewhere discovered that a set of proteins called ESCRT-III delays or even prevents necroptotic cell death by knitting the broken membrane into bubbles. The cell then sheds these bubbles, leaving an intact membrane and a viable cell. Gong also did experiments with tissue from kidneys used in transplants, showing that even though MLKL was switched on, the cells didn't die, and this protection was accompanied by an increase in ESCRT-III proteins. This is a first hint that our findings have relevance to transplantation.
We still have a long way to go to apply these findings clinically. So far, our experiments have been only in cells, so we haven’t shown the process in tissues and whole organs. And we still don’t know the details of how MLKL damages the cell membrane, or how and why the cell "decides" to recruit ESCRT-III to repair the holes and delay its death.
You can read more about the findings in a recent issue of Cell.
There's this wonderful Chinese legend that we think captures the spirit of our discovery. According to the legend, in ancient times a titanic battle between gods destroyed one of the pillars holding up the sky. The pillar's collapse opened up a hole in the heavens cracking the Earth and causing great devastation — fires, floods and marauding animals. The goddess Nüwa, who had first created humans, took pity on them and using colored stones, patched up the sky, giving it the many hues it has today. She also restored the pillars, controlled the floods, quenched the fires and drove away the wild animals.
Our research has discovered a biological equivalent of Nüwa.
1. Karam JA, Hsieh JT (2009) Apoptosis in Carcinogenesis and Chemotherapy: Apoptosis in Cancer pp 25-50.






