St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
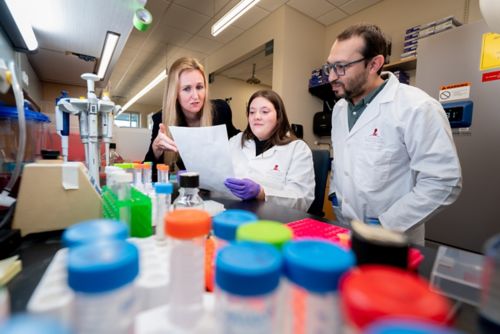
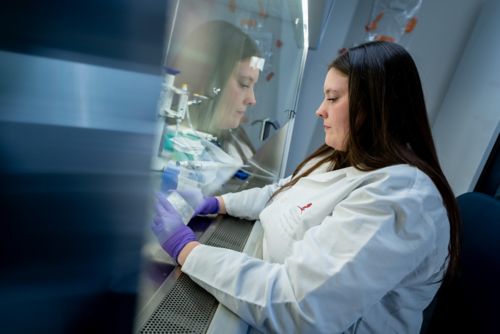
Caitlin Zebley Lab
Examining epigenetic mechanisms of T cell differentiation to advance cellular therapies
About the Caitlin Zebley Lab
Over the years, therapeutic approaches for children with cancer have expanded to the cellular level, while research has led to a better understanding of how we can bolster the body’s own immune response as a treatment. This approach, known as immunotherapy, often relies on the functional persistence of T cells for therapeutic efficacy. While T-cell-based therapies offer new possibilities in targeted treatment, its effectiveness improves as we learn about the body’s T cells, how they undergo differentiation, and how we can use epigenetic engineering approaches to modify T cell differentiation status to make them better able to fight against cancer. Our laboratory studies how T cells develop and mature so we can improve targeted cellular therapies that benefit pediatric patients with cancer.
Our research summary
Cellular differentiation – the pathway and process through which cells develop from an unspecialized state into specialized cells with a particular function – is a crucial process that dictates a cell’s role and function. In T cells, the differentiation process not only determines function but how these cells interact with tumor cells and how they can be used against tumor growth. Examining mechanisms of T cell differentiation is the central component of our work, a focus that expands our understanding of how these mechanistic properties can be harnessed to improve cellular therapies.
Overcoming T-cell exhaustion
Despite the promise of immunotherapy, a known limiting factor of durable therapeutic success is T-cell exhaustion – a state in which T cells lose their protective capacity due to prolonged exposure to an antigen. Our past and ongoing research demonstrates that it is possible to overcome these obstacles of exhaustion and engineer T cells with specific epigenetic programs that instill disease-relevant, long-lived immunological properties. Our examination of T-cell differentiation focuses on restricting the terminal exhaustion of CD4 and CD8 T cells to bolster immunotherapeutic effects and strengthen effective, long-term cellular therapies.
Defining epigenetic regulators of T-Cell stemness
Furthering our study of T-cell differentiation and exhaustion is our work to define the epigenetic regulators that restrict antitumor immunity during prolonged antigen exposure. Our laboratory examines mutations that occur during the premalignant state of clonal hematopoiesis (CH).
Our goal is to understand how disruption of key CH-associated epigenetic regulators impact T-cell differentiation and how we can target these regulators to block the progression of T cell exhaustion. We are working to design an ideal CD8 T cell population for adoptive transfer that is proliferative and maintains effector potential that provides a long-lasting anti-tumor response. My goal is to continue to expand my research program to implement our laboratory findings in future cellular therapies that directly benefit patients with catastrophic disease.
Publications
Contact us
Caitlin Zebley, MD, PhD
Assistant Member
Department of Bone Marrow Transplantation and Cellular Therapy
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS