St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Jun J. Yang Lab
Uncovering how genetics can be used to tailor cancer therapy in children
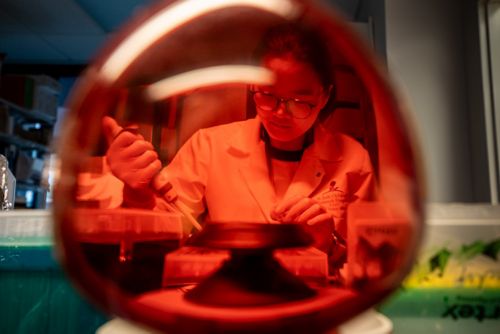
About the Yang Lab
Leukemia is the most common pediatric cancer, but it exhibits profound differences from patient to patient. Individuals vary widely with regard to risk of developing the disease, and propensity for developing drug resistance or treatment toxicity. Our laboratory uses a genomic-based approaches to decipher the mechanisms that drive these differences. Our goal is to determine how variations in genetic makeup can be leveraged to predict and improve response to leukemia therapy in children.
In the news
The St. Jude Postdoctoral Leadership Council and the Postdoctoral Association have selected Jun J. Yang, PhD, vice chair, Pharmacy and Pharmaceutical Sciences, as the 2023 Mentor of the Year.
In the news
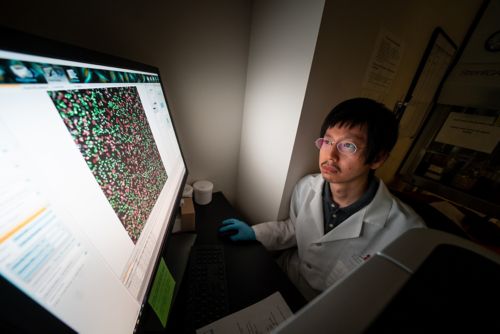
Bioinformatics Research Scientist, Zhenhua Li, PhD, used whole-genome sequencing and RNA-seq to characterize the genomic landscape of acute lymphoblastic leukemia from 295 patients with Down syndrome. This work highlights the distinctive leukemia biology, including 15 unique subtypes, and provides opportunities to explore targeted therapy for this specific population.
In the news
Jun J. Yang is being honored at AACR with the Waun Ki Hong Award for his inspiring contributions to genomic studies dedicated to analyzing therapeutic response rates in multiethnic pediatric acute lymphoblastic leukemia patient populations, which have resulted in the identification of a large number of genomic loci responsible for driving therapeutic response variability. These findings are now being leveraged to predict treatment efficacy and toxicity in pediatric cancer populations. Read about it.
In the News
Jun J. Yang supervised a study involving targeted sequencing of over 5,000 patients with Philadelphia chromosome-like ALL (Ph-like ALL), identifying a key regulatory germline variant in GATA3. This variant caused global re-shaping of chromatin, positive regulation of the ALL oncogene CRLF2, and potentiated the JAK-STAT oncogenic effects during leukemogenesis. Read the full work here. Noncoding genetic variation in GATA3 increases acute lymphoblastic leukemia risk through local and global changes in chromatin conformation.
In the news
Postdoc Xujie Zhao led work published in JNCI (2022) illustrating that for acute lymphoblastic leukemia (ALL), non-coding risk variants in the gene ARID5B function by modulating cis-regulatory elements at this locus. Learn more by reading the article. Molecular Mechanisms of ARID5B-Mediated Genetic Susceptibility to Acute Lymphoblastic Leukemia.
In the news
Postdoc Yizhen Li (PhD) served as first author of a study that included sequencing over 6,100 children with acute lymphoblastic leukemia (ALL). She identified germline RUNX1 variants and other mutations responsible for predisposition to childhood ALL. The work was published in JCI in June, 2021. Germline RUNX1 variation and predisposition to childhood acute lymphoblastic leukemia.
In the news
Postdoc Shawn Lee (MD) worked to assemble a large multi-national, multi-ethnic cohort of children with acute lymphoblastic leukemia (ALL) and studied the impact of genetic ancestry on the somatic genomics and survival outcomes of childhood ALL. This work highlights the contribution of genetic ancestry to racial disparities in ALL therapy, and demonstrates the importance of racial/ethnic considerations in future ALL research and treatment. Association of Genetic Ancestry With the Molecular Subtypes and Prognosis of Childhood Acute Lymphoblastic Leukemia.
In the news
Former postdoc Jianzhong Hu, in collaboration with the Department of Chemical Biology and Therapeutics at St. Jude, developed a novel chemical technology serving as a targeted-therapeutic approach that may benefit patients with aggressive leukemia. Read the paper.
In the news
DNA isn't destiny, but genetic predispositions do underlie many cancers. St. Jude scientists have gained a nuanced understanding of cancer predisposition and are learning more to help personalize patient therapies. Learn more. #StJudeOn
Our research summary
Driven by observations of inter-individual variations in patients with pediatric leukemia, our research is dedicated to understanding how genetic variation dictates this diversity. We take an agnostic and genome-wide view, to explore genetic factors across the entire human genome in large cohorts of patient with different phenotypes (e.g., drug resistance or toxicity). From there, we identify specific genes related to these traits, and interrogate them to understand the mechanism linking a particular genetic variant to a particular phenotype. We are particularly proud of our close collaborations with clinical investigators and the global diversity in pediatric leukemia we study.
Using pharmacogenomics to develop novel therapies for pediatric leukemia
Although the cure rate of pediatric leukemia is high, this was achieved by brute-force approach using cytotoxic chemotherapy for decades. We are leading efforts at St. Jude to develop the next generation of leukemia therapy with surgical precision, leveraging genetic insights developed over the past 10 years. Studying 1000+ leukemia patients across the US, we are examining their pharmacotype and profiling genomes at the same time. Our aim is to construct a gene-drug connectivity map to identify biomarkers and predictors of patients’ response to novel leukemia drugs. We have already started developing a biomarker-informed clinical trial for pediatric T-ALL based on this work and look forward to applying this approach to other subtypes of ALL.
Identifying the genomic drivers of chemotherapy-induced liver injury
The liver is a vital organ that has many important roles in the metabolism of nutrients and drugs. Liver injury is one of the most common drug toxicities and a major cause of failure for investigational drugs. We have previously identified pharmacogenomic associations with liver injury during chemotherapy in children and are actively investigating mechanistic details of this toxicity. We seek to uncover insights such as, which cells in the liver are damaged by which drug, what molecular processes are affected by each medication and how exposure to different drugs influences interactions between different type of cells in the liver. In collaboration with the Department of Computational Biology and the Center for Spatial Omics at St. Jude, we use single-cell and spatial-omics technologies to dissect the biology of drug liver toxicity.

Using pharmacogenomics to predict treatment toxicity
The drugs currently used to treat pediatric leukemia are highly efficacious, but with profound adverse effects. It is important that we understand the underlying causes of toxicity and try to mitigate this deleterious response in patients. Again, our team takes a genomic approach – comparing patients with vs without toxicity in genome-wide scans to identify specific variants associated with the side effects. Our group discovered genetic polymorphism in the NUDT15 gene that puts children at a dramatic risk of myelosuppression following treatment of an anti-leukemia drug called thiopurine. By elucidating the molecular mechanism of how NUDT15 modulates thiopurine metabolism, we developed ways to use pharmacogenomics to individualize their therapy, reducing associated toxicities by almost 90%. This work has led to the change of thiopurine drug label by the Food and Drug Administration. We are currently exploring pharmacogenomics of other pediatric cancer drugs.
Determining genetic risk factors for developing leukemia
Fundamental to our work is the understanding that children are at varied risk for developing leukemia. We use genome wide studies to explore the genetic variants that drive the formation of leukemia. Our laboratory, in collaboration with other investigators at, and beyond, St. Jude, has developed cohorts of children with leukemia, and their healthy counterparts. We compare the genetic makeups of each population and identify putative risk factors – genes enriched in afflicted children. Additionally, we work to identify rare families with multiple cases of leukemia, suggesting highly penetrant genetic risk factors. We utilize engineered mouse models to manipulate genes of interest identified in these studies and investigate the resulting hematopoietic phenotypes. Ultimately, our goal is to understand the genetic basis for susceptibility to pediatric leukemia.
Contact us
Jun J. Yang, PhD
Member and Vice Chair
Department of Pharmacy and Pharmaceutical Sciences
MS 313, Room I5104
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS