St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude is committed to leveraging its assets to accelerate progress and maximize impact for children in Memphis and around the globe with an acute focus on fundamental science, childhood cancer, pediatric catastrophic disease, global impact, and workforce and environment. St. Jude has, and will continue to, significantly influence the way the world understands and treats childhood cancer, sickle cell disease, neurological disorders, and infectious diseases.
Explore our research
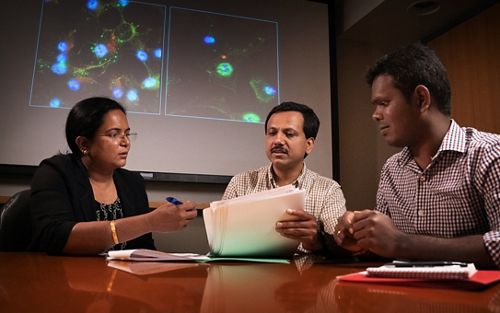
The St. Jude environment facilitates interaction among laboratory scientists and clinical investigators, promoting the translation of new findings from the lab to the clinic and communicating clinical problems to laboratory scientists for further investigation. Our 22 academic departments are home to more than 120 fundamental and translational research labs that bring the ‘bench to the bedside,’ ensuring that patients treated at St. Jude benefit fully from advances in our understanding of pediatric catastrophic diseases and their treatment.
Explore the work of our lab-based investigators by searching for a PI/Faculty name.
What sets St. Jude apart?
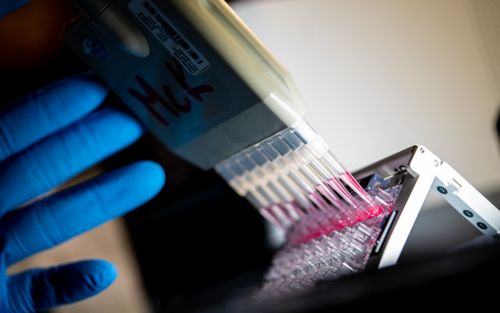
Unrivaled shared resources
St. Jude has over 20 core facilities and research resources that provide expertise and cutting-edge technologies to support collaborative work across the institution.

Careers & training
Answer your calling at St. Jude
St. Jude is a community of diverse faculty, staff, and trainees who strive to ask bold questions, create innovative solutions, and strengthen the robust scientific enterprise. St. Jude investigators have the freedom to focus on making big discoveries, backed by extraordinary resources and support teams.
Progress: A Digital Magazine
Sharing stories of impact and discovery across the St. Jude research enterprise.
A new St. Jude study uncovers genetic factors behind pediatric thyroid cancer risk.
See how tools like mitoedit and NETBID reveal mitochondrial DNA (mtDNA) ties to diseases such as acute lymphoblastic leukemia
Watch how St. Jude visual storytellers use artistry to support scientific discovery
St. Jude clinicians collaborate with fellow palliative care experts to advocate for bringing palliative care to patients with sickle cell disease.
An extraordinary academic institution
Learn how a degree from the St. Jude Children’s Research Hospital Graduate School of Biomedical Sciences can help you further your science and make a difference.
With world-class basic and translational research, mentorship from internationally renowned faculty and exceptional support and resources, our degree programs offer a unique experience for all our students.

Memphis, TN, 38105-3678 USA GET DIRECTIONS