St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Roussel Lab
Understanding the molecular basis of malignant pediatric brain tumors and developing preclinical pipelines to evaluate therapeutic approaches.
About the Roussel Lab
Our lab studies some of the most aggressive, and difficult to treat, forms of pediatric brain tumors. We have developed a research pipeline that integrates molecular characterization, model development, and preclinical and clinical strategy. Our long-term goal is to find new, and improve existing, therapies for patients with malignant brain tumors.

Our research summary
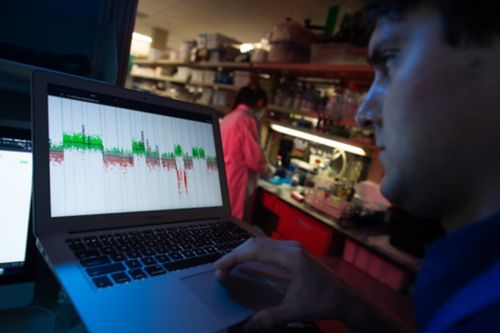
Our laboratory uses an integrated and multidisciplinary state of the art approaches including extensive molecular and immunologic characterization of malignant pediatric brain tumors to understand the etiology of disease and identify drivers of tumor development. This, in turn, has allowed us to develop several accurate mouse models of medulloblastoma (MB) that recapitulate human disease and facilitate translational experiments. We have also generated a large cohort of orthotopic xenografts of primary tumor samples from patients treated at St. Jude that are currently used to validate the efficacy of known drugs and targeted therapies in pre-clinical trials. Our work continues to evolve as we partner with internal and external collaborators through interdisciplinary research consortia.
Modeling the most aggressive forms of pediatric brain tumors
In order to understand the development and resilience of malignant pediatric brain tumors, we need access to model systems that recapitulate human disease. Built on our understanding of cell cycle regulation and MYC family signaling pathways, we have developed several models of MB representing the most aggressive forms of disease. Subsequently, we generated a mouse model with endogenous, CRISPR-driven, overexpression of MYC that has facilitated additional questions around transcriptional-targeting therapies and epigenetic regulation. Our next step is to generate these models in human-based cell systems for even greater translational relevance. Critically, my laboratory has generated a cohort of molecularly conserved and fully characterized patient-derived orthotopic xenograft (PDOX) models of primary tumor samples acquired from St. Jude patients. These models are essential to understand the heterogeneity of pediatric brain tumors and to develop effective preclinical strategies to inform clinical trial design.

Targeting transcription factors that drive medulloblastoma
Transcription factors have been considered “undrugable” but recent development of molecules including PROTACs and Molecular Glues provide a unique opportunity to directly degrade these proteins that do not have pockets targetable by drugs. In collaboration with experts in chemical biology, structure biology and molecular biology, we are targeting MYCN, GFI1 and GFI1B, transcription factors; all factors required for medulloblastoma development. Such degraders will be validated in mouse and human medulloblastoma models using our pre-clinical pipeline.
Epigenetic regulation of pediatric brain tumors
In addition to amplification of oncogenes and mutation of tumor suppressors, genetic alterations in epigenetic regulators account for the majority of genetic perturbations in Group 3 and Group 4 MB. An altered spectrum of epigenetic regulators and chromatin modifiers, resulting in aberrant patterns of histone lysine methylation, further distinguishes subgroups of MB. Using unbiased, genetic-based screening approaches, we have identified putative epigenetic regulators of tumorigenesis in MB and are currently working to define their molecular mechanisms and functional roles. Our laboratory collaborates with experts across St. Jude, leveraging informatics analysis, structural modeling, and functional genomics to uncover drivers and vulnerabilities in MB.

Pre-clinical modeling and therapeutic development for pediatric brain tumors
Ultimately, our laboratory is interested in developing new approaches and optimizing current strategies to more effectively treat pediatric brain tumor patients. We have established collaborative research teams with clinicians, pharmacokineticists, chemical biologists and statistical experts to create an integrated pipeline from molecular analysis to clinical trial design and launch. In previous work, high throughput screening of a library of FDA-approved drugs identified several chemotherapeutic compounds that have been advanced into ongoing clinical trials for the treatment of MYC-driven MB. Utilizing a fully characterized cohort of PDOX models, targeted therapies and craniospinal radiation protocols are also being optimized and explored for MB and ATRT.
Learn more
Selected Publications
Contact us
Martine F. Roussel, PhD
Tumor Cell Biology MS350
St. Jude Children’s Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS