St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Paul Northcott Lab
Leveraging unparalleled clinical cohorts & innovative experimental systems to resolve the mechanisms underlying malignant embryonal CNS cancers
About the Northcott Lab
Medulloblastoma and pineoblastoma are heterogeneous embryonal central nervous system (CNS) tumors arising in early life. Current therapeutic approaches are successful in only a portion of cases, and survivors often face severe long-term challenges because of current treatments.
To improve the efficacy and safety of intervention, a deeper understanding of the biological and clinical heterogeneity of these tumors is required. We leverage extensive expertise in multi-omics, bioinformatics, in vivo and ex vivo models, and functional screens to decipher the developmental, cellular, and mechanistic basis of aggressive pediatric brain cancers and identify novel treatment targets.

Our research summary
Our lab applies bold, innovative strategies to advance knowledge of embryonal CNS tumors and disrupted neurodevelopment. We study genetic dependencies and preclinical models for treatment development, leverage liquid biopsy for monitoring disease and resolving resistance mechanisms, and use translational genomics for improving outcomes of children affected by malignant brain tumors.
Embryonal CNS tumors
Our lab utilizes translational genomics, discovery-driven bioinformatics, functional validation, and neurodevelopmental studies to decipher the heterogeneity and cellular origins of embryonal CNS tumors.
Tumor subgroups have unique molecular landscapes corresponding to clinical response and outcomes.. We are pioneering multi-omic single cell approaches on large cohorts to describe intratumoral heterogeneity and identify molecular and genetic mechanisms of these devastating cancers.

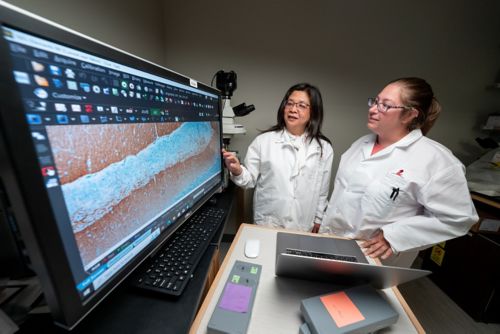
Single-cell sequencing of individual cells from a particular tumor sample enables better resolution to infer how alterations arose over time in heterogenous cell populations. We compare tumor cell profiles to normal developmental atlases to retrace developmental origins and resolve cellular hierarchies to describe the acquisition of tumorigenic properties and subsequent differentiation. This knowledge will enhance disease modeling approaches and help disclose potential therapeutic vulnerabilities that are masked in the bulk tumor.
Disrupted neurodevelopment in pediatric brain tumors
Comparisons between tumor and normally developing cells can identify the cell of origin of cancer subtypes to pinpoint where and how tumorgenic processes arise.
Many medulloblastoma tumors feature driver mutations in regulatory genes including chromatin modulators or transcription factors. This suggests disrupted developmental gene expression is a fundamental feature of medulloblastoma pathogenesis. However, how chromatin/transcriptional machinery defects contribute to medulloblastoma remains poorly defined.
Our lab is investigating the consequences of medulloblastoma-associated chromatin modifier mutations in developmental context using CRISPR-mediated genetic perturbation, targeted protein degradation, genetically engineered mouse models, and integrative chromatin state profiling. Studies of high priority candidates reveal prominent themes in chromatin deregulation, such as enhancer hijacking through structural variations altering 3D genomic architecture.

Genetic dependencies and preclinical model development
Functional validation of candidate driver genes, or mutations causing these devastating cancers, has the potential to reveal unique molecular mechanisms of pathogenesis. Dependency studies identify putative vulnerabilities in designing targets for treatment.
We leverage predictive models and genetic interaction studies to prioritize targets and test novel compounds for efficacy in preclinical models. Promising preclinical discoveries can be tested in clinical trials with collaborators to develop safer and more effective treatment options for patients and families.
Liquid biopsies to monitor disease and resolve resistance mechanisms
Efforts to improve outcomes in children diagnosed with medulloblastoma have been hampered by the lack of sensitive biomarkers to stratify treatment response and predict relapse. Tumor-derived cell-free DNA collected from cerebrospinal fluid (CSF) of patients via liquid biopsies can detect and track tumor-specific genomic alterations.
We have developed state-of-the art sequencing and bioinformatics methods to identify tumor signatures via liquid biopsies collected from children enrolled on clinical protocols. Applications include capturing epigenetic profiles of tumor evolution during treatment that can predict recurrence or failure to respond to interventions.
This work is leveraged across clinical collaborations to translate biological insights into tools for diagnosis, risk-stratification, and interpretation of trial outcomes.
Using translational genomics to improve clinical practice
We aim to translate our preclinical discoveries through clinical collaborations to improve diagnosis, stratification, and treatment options for patients and families. In collaboration with clinicians and scientists within the Neurobiology and Brain Tumor Program of the St. Jude Comprehensive Cancer Center, we are creating in depth molecular profiles for patients enrolled in St. Jude and Children’s Oncology Group medulloblastoma trials.
By correlating gene mutations, structural variants, copy-number alterations, transcriptomes, proteomes, and cancer subgroup/subtype status with detailed clinical trial data, we aim to improve prognostics and precision medicine opportunities.
These strategies include identifying risk groups, tailoring the intensity of therapy based on likely responses, and pinpointing who would benefit from molecularly targeted therapies. We also describe how tumors evolve in response to treatment for designing more effective therapies to reduce recurrence and improve future outcomes for these children.
Northcott Lab selected publications
Contact the Northcott Lab
Paul A. Northcott, PhD
Endowed Chair in Molecular Neuro-Oncology
Director, Center of Excellence in Neuro-Oncology Sciences (CENOS)
Member, Department of Developmental Neurobiology
Member, Neurobiology & Brain Tumor Program
MS 325

Memphis, TN, 38105-3678 USA GET DIRECTIONS
