St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Kiel Neumann Lab
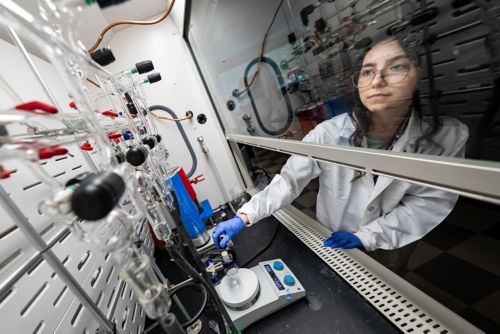
Developing radiopharmaceuticals for a theranostics-based approach to neurological and oncological conditions and exploring diagnostics for infectious diseases
About the Neumann Lab
In the management of catastrophic illness and infection, the ability to rapidly and accurately diagnose and treat disease influences outcomes. The use of radiopharmaceuticals – pharmaceutical drugs that contain radioactive isotopes – offers both diagnostic and treatment potential. Our laboratory develops and studies radiopharmaceuticals that can be used as both a diagnostic test and a therapeutic intervention in an approach called theranostics. By better understanding how a theranostics-based approach leads to better diagnoses and targeted treatments using radiopharmaceuticals, we aim to improve outcomes in conditions related to neurology and oncology. Our desire to provide accurate, non-invasive diagnostic tests extends our pioneering work to the infectious disease space.

Our research summary
Radiopharmaceuticals can be used as theranostic agents, in which the radiopharmaceutical is simultaneously a diagnostic test and a therapeutic intervention. In our research, we develop radiopharmaceuticals tagged with a positron emission tomography (PET) isotope, which controls whether the radiopharmaceutical has a diagnostic or therapeutic ability. Everything we do is a matter of switching that tag to make the radiopharmaceutical a targeted diagnostic or therapeutic agent. In addition, radiopharmaceuticals can be employed to study when a traditional, nonradioactive therapeutic strategy is likely to be successful in a given disease state.
Our work concentrates on three areas of study that span neurological and oncological conditions and infectious diseases.
Defining therapeutic windows for neurological care
Reactive oxygen and nitrogen species (RONS) are molecules with a brief biological half-life that facilitate messaging and other basic functions in the brain. In normal states, the body can regulate the presence of RONS, but in conditions like stroke or chronic pathological disease like Alzheimer’s, RONS accumulates and leads to oxidative stress due to a prolonged defense mechanism imbalance. In this state, various conditions such as axonal loss, neurotoxicity and necrosis of brain cells occur, all of which lead to cognitive dysfunction.

Oxidative stress has an early implicative role in many neurological disorders but discovering when RONS is present has practical challenges. The current gold standard for detecting RONS is tissue extraction, which is not a suitable approach in humans. Because of this practical challenge, it is unknown at what point the RONS is present, which limits viable targets for treatment.
To address this limitation, our aim is to improve antioxidant therapeutic strategies by using a non-invasive test to determine when oxidative stress has a relevant role in disease pathology (either early, late, or not at all).
We use isotopically labeled antioxidants, which are injected into preclinical models and imaged with preclinical PET scanners to define therapeutic windows in both acute and chronic disease conditions. Once we are able to define therapeutic windows, we can intentionally design our antioxidant strategy, which removes the PET isotope from the radiopharmaceutical so the remaining pharmaceutical acts as a therapy for oxidative stress.
We also conduct collaborative work on oxidative stress markers in survivors of Hodgkin lymphoma. By collaborating with Kevin Krull, PhD, and Asim Bag, MD, we assess the impact of oxidative stress from treatment approaches that may lead to neurodegeneration over time. The goal is to understand at what point cognitive interventions could be implemented to preserve neurocognitive function in the future.
Developing novel theranostics for pediatric glioma
Our work in the oncology field focuses on improving disease outcomes by developing novel theranostic agents for use in the diagnosis and treatment of pediatric high-grade gliomas, such as medulloblastoma, diffuse midline glioma (DMG), and glioblastoma multiforme (GBM). One of the main obstacles in treating patients with these devastating brain tumors is the inefficiency in which pharmaceuticals are able to get to the tumor, as the brain is naturally protected by a layer of cells called the blood brain barrier. We can use radiopharmaceuticals to noninvasively determine whether a molecule is able to cross the blood brain barrier and to what degree it reaches and stays within the tumor. We can then change the isotopic label that we used for imaging to a label that has useful therapeutic properties. In this way, we can use theranostics to expand the catalogue of treatment options available for patients who are in desperate need of new strategies to treat these devastating tumors.
Using a PET imaging agent to diagnose bacterial infections
Another area of our research that seeks to provide a non-invasive, reliable alternative to current diagnostic tests reaches into the infectious disease arena.
The current gold standard for diagnosing deep-seated infections is biopsy, but biopsies are prone to sampling error that can lead to false positives or negatives.

Other imaging modalities like computed tomography (CT), magnetic resonance imaging (MRI) or even fluorodeoxyglucose positron emission tomography (FDG-PET) cannot accurately differentiate sterile inflammatory processes from deep-seated bacterial infections.
But what if we developed a PET imaging agent specifically for bacterial infections? Our goal is to provide a diagnostic test using PET imaging for patients with deep-seated infections that are difficult to diagnose as an infection versus another inflammatory process. Implicit in this specific test is the ability to rapidly determine whether a specific antibiotic is working or in the case of a drug-resistant bacteria, failing. In this way molecular imaging can deliver precise and accurate data to inform clinical decision.
At St. Jude, this becomes imperative in patients with sickle cell disease. Patients often present in a pain crisis, but how can clinicians be sure whether the patient is experiencing a vaso-occlusive episode or an infection such as osteomyelitis? Use of this PET imaging agent may be able to determine the most effective treatment by allowing clinicians a definitive diagnosis that guides the correct therapeutic decisions.
Our work in this area is bolstered by collaborations with Jason Rosch, PhD, who develops the murine models to emulate osteomyelitis infections in patients with sickle cell disease, , as well as Amanda Green, MD and Dr. Josh Wolf, who routinely care for these patients.
Across all our research areas, the use of shared resources and access to state-of-the-art imaging technology, such as PET/CT, PET/MRI, high-field MRI allow us to ask new questions and address challenges in the field of radiopharmaceutical research.
Being in such close collaboration with the molecular imaging core (MIC) provides us with a cyclotron to produce radioisotopes and gives us access to shielded hotcells to conduct radiochemistry. The expertise within the MIC also provides us guidance as we navigate the vast regulatory realm of our research.
As our research advances, our desire to improve outcomes across acute and chronic disease states, for both pediatric and adult neurological and oncological conditions and infectious diseases, continues to be our driving force.
Selected publications
Contact us
Kiel Neumann, PhD
Assistant Member. St. Jude Faculty
Department of Radiology
MS220, Room I3120A
St. Jude Children's Research Hospital
Follow Us

Memphis, TN, 38105-3678 USA GET DIRECTIONS