St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Charles Mullighan Lab
Characterizing the genomic drivers of leukemia and treatment failure
About the Mullighan Lab
There are constellations of inherited and acquired genetic changes that drive acute lymphoblastic leukemia and related disorders. Our lab works to identify these changes and define their molecular mechanisms. We leverage genomic technologies and large patient cohorts, along with experimental and preclinical modeling. Our ultimate goal is to translate our discoveries into advances in cancer diagnosis and therapy.
Our research summary
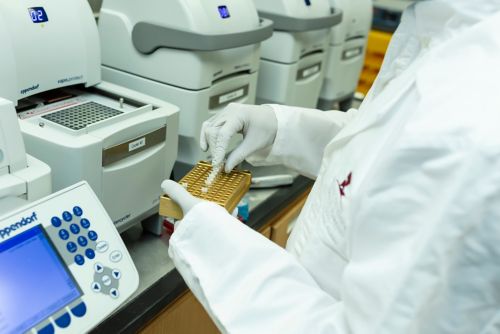
Our laboratory uses high-end genomic studies to better understand the pathogenesis of acute lymphoblastic leukemia (ALL) and other high risk leukemias. The integrated research approach we take involves large-scale, multimodality genomic profiling of large patient cohorts to identify constellations of genetic changes. This is complemented by the development of experimental models that rigorously probe mechanism to understand how genomic alterations drive tumorigenesis and treatment response. We then translate these findings into new diagnostic tools and therapies to improve the cure rates for ALL and related cancers.
Our laboratory makes all our reagents, models, and data available to the research community. We have one of the world’s largest repositories of derived xenografts of patients with ALL through our PROPEL repository, with more than 300 samples.
Molecular classification of ALL
The lab began in the field of genomic interrogation of ALL and continues to lead studies defining the genetic basis of ALL as well as other high-risk leukemias. The genomic profiling studies in our laboratory encompasses sequencing and analysis of very large cohorts of ALL and AML, to more narrowly focused studies, for example examining the genetic basis of relapse, lineage ambiguous leukemias, and response to hew therapeutic agents such as immunotherapy. These studies span the age spectrum, and involve close collaboration with childhood and adult cooperative groups, including the Children’s Oncology Group (COG) in projects support by the NCI’s Molecular Profiling to Predict Response to Treatment program and Gabriella Miller Kids First program. These projects are focused on determining the basis of relapse in standard risk B-ALL, and T-ALL. Each project involves sequencing 1,500 cases using whole genome and RNA sequencing, to discover the genomic differences between patients who relapse from ALL. when they were considered standard risk.
Ph-like ALL
Our laboratory co-discovered BCR-ABL1-like (Ph-like) ALL, one of the most common and high-risk subtypes of ALL. We previously led the efforts to describe the diverse genomic landscape of the disease and its prevalence across the age spectrum, define the potential for inhibition of kinase signaling in ALL, and establish new mouse models of Ph-like ALL that show sensitivity to kinase inhibition. These findings have had a global impact, leading to revision of the molecular classification of ALL by the World Health Organization, multiple trials evaluating the potential of TKI therapy, and naming of the discovery of Ph-like ALL as one of the most important advances in the field of hematology in 2015.
High-risk ALL characterization
Our laboratory continues to have a major interest in defining the genetic basis of poorly understood, high-risk forms of leukemia and translating these findings to new mechanistic and therapeutic approaches. Our research in this area includes projects on lineage-ambiguous leukemias. We previously conducted the first genome sequencing study of any pediatric malignancy when we defined the genomics of early T-cell precursor leukemia using whole genome sequencing. Our laboratory has gone on to characterize other lineage-ambiguous leukemias, the results of which have had important implications for leukemia diagnosis and classification and have led to additional research examining the cells of origin and the roles of these alterations in leukemia pathogenesis.
Another line of ALL characterization in our laboratory involves acute erythroleukemia, which is characterized by excessive erythroblasts in the bone marrow, a degree of similarity to acute myeloid leukemia (AML) and myelodysplasia (MDS), and dismal outcome. Our research in this area demonstrated that the genome features of acute erythroleukemia are distinct from AML and MDS. In addition, our research illuminated the potential for targeting multiple pathways for treatment and demonstrated the roles of specific combinations of genomic aberrations in defining disease lineage and phenotype.
?wid=500)
Clonal evolution and mechanisms of treatment failure
Our laboratory has led numerous studies examining the relationship of genetic variegation, clonal evolution in relapse in ALL, and the mechanisms by which relapse-enriched mutations drive drug resistance. We published a seminal study on ALL – and later confirmed for most cancer types – showing that there is partial sharing of the genetic alterations between the predominant diagnosis and relapse clones, and that relapse-enriched mutations could be backtracked to minor clones in most cases. We continue our research into clonal evolution and treatment failure, using genomic approaches to study novel immunotherapy and CAR-T treatments.
Germline predisposition to ALL
Our laboratory has identified many of the genes leading to the development of ALL predisposition genes, and we have characterized the leukemogenic effects of these alterations. Specifically, we have studied germline mutations in TP53 and IKZF1 and continue to investigate the mechanistic basis for germline mutations in ALL.
Leukemia microenvironment and drug resistance
Our laboratory has active research projects focused on the interactions of leukemia cells with the microenvironment as a mechanism of drug resistance, building upon our earlier research on alterations of IKZF1 in high risk B-ALL. Ongoing studies using in vitro and in vivo models of B-ALL examine the general importance of the interaction of ALL cells with the bone marrow niche as a mechanism of quiescence and drug resistance. We are currently involved in two projects through Alex’s Lemonade Stand to model these interactions between ALL cells and the bone marrow niche as well as study the single-cell profiling of ALL samples in the microenvironment.

New therapeutics
The research in our laboratory further extends to potential new therapeutic approaches for ALL, focusing on the ubiquitin ligase machinery to target proteins or conventionally intractable targets for proteosome degradation. One project along this line of research inquiry involves the use of proteolysis-targeting chimeras directed at the JAK-STAT family of proteins in Ph-like leukemia. A second project explores the use of molecular glues to degrade and tackle some of the most intractable targets in leukemia and medulloblastoma as well as fusion oncoprotein-driven tumors.
In addition, through our participation in a Cancer Moonshot-related initiative, our laboratory is part of a multi-institutional study investigating aimed at understanding the biology of the NUP98 fusion oncoprotein to develop new therapeutic strategies for cancer.
Find out more
Selected Publications
Contact us
Charles G. Mullighan, MBBS (Hons), MSc, MD
Pathology
MS342
St. Jude Children's Research Hospital

Memphis, TN, 38105-3678 USA GET DIRECTIONS



