St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Chia-ho Hua Lab
Leveraging the proton therapy process’s key components for accuracy and precision
About the Chia-ho Hua Lab
The field of radiation oncology is moving toward maximizing the therapeutic ratio with particle therapy and advanced image guidance, as well as predictive models of tumor response and normal tissue effects in the era of precision medicine. Our research group strives to develop novel methodologies and apply cutting-edge imaging technologies to increase the targeting accuracy of proton therapy and build pediatric organ-specific models of radiation treatment effects to guide clinical decision-making.

Our research summary
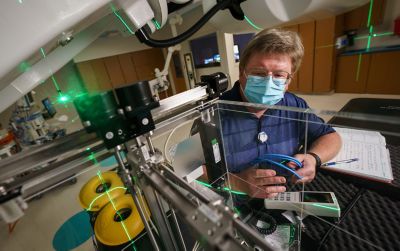
Improving targeting accuracy of proton therapy
The Hua lab focuses on the proton therapy process’s key components to increase its accuracy and precision. Our research group has optimized and developed a clinical workflow for pediatric magnetic resonance (MR) simulation. We designed the robotic cone-beam computed tomography (CBCT) for image-guided proton therapy and developed methodology for more accurate proton therapy planning with stopping-power imaging from spectral CT. Through our concerted efforts, we advanced artificial intelligence-driven adaptive proton therapy to address on-treatment changes in tumor volume and normal anatomy. Additionally, we assessed the tumor and organ motion with our novel 4D MRI technique and predicted the interplay effect with scanning proton beams. Our research has led the practice guideline development in pediatric image-guided radiotherapy on behalf of the Children’s Oncology Group.
Imaging radiation effects on pediatric brain
To better understand the radiation dose effects on a normal pediatric brain and their subsequent relationship to clinical sequelae, our research group has studied serial MRI and diffusion tensor imaging on pediatric brain tumor patients who received radiation therapy. Our track- and connectome-based analyses discovered the differences in radiation sensitivity of brainstem fiber tracts in children, the accentuating effect of surgery on radiation injury, and the patterns of white matter tract integrity and neurocognitive performance.

Pediatric normal tissue complication modeling
A valuable contribution of our research group to radiation oncology is the development of quantitative radiation dose-volume effect models for predicting the risk of pediatric organ-specific toxicity after radiotherapy. The investigated clinical endpoints include flat bone growth, height reduction, scoliosis, hearing loss, growth hormone deficiency, radiation pneumonitis, and premature ovarian insufficiency and failure. Our research guides the radiation oncology community in maximizing tumor coverage while minimizing the normal tissue complication risk.
Publications
Contact us
Chia-ho Hua, PhD, FAAPM
Member, Radiation Oncology
Director of Medical Physics Research
Department of Radiation Oncology
MS 210, Room I3133
St. Jude Children's Research Hospital
Follow Us

Memphis, TN, 38105-3678 USA GET DIRECTIONS