St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Center of Excellence in Neuro-Oncology Science
Suzanne Baker Lab
Deciphering the pathogenesis and therapeutic vulnerabilities of pediatric high-grade glioma
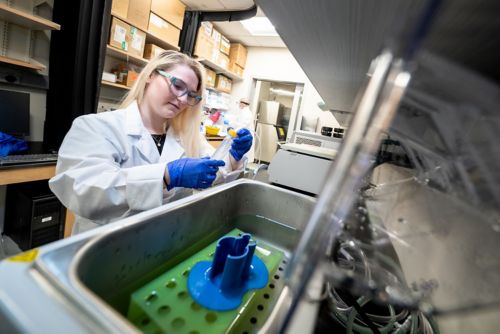
About the Baker Lab
Brain tumors are the leading cause of cancer-related death in children, and pediatric high-grade glioma (pHGG) is one of the most devastating brain tumors of childhood. Our laboratory analyzes pHGG patient tumor samples and develops genetically engineered and patient-derived models for mechanistic approaches to understand the connections between tumorigenesis, chromatin regulation and developmental signaling pathways in the brain. Our goal is to enhance the mechanistic understanding of HGG and to identify therapeutic vulnerabilities so that our research can be translated to clinical impact for patients.

Our research summary
The genomic landscape of pHGG reveals a spectrum of mutations closely associated with patient age and tumor location, highlighting a critical interplay between developmental context and gliomagenesis in children. Our group co-discovered histone H3 mutations in pHGG, identifying H3 K27M mutations in nearly 80% of diffuse intrinsic pontine glioma (DIPG), and lower frequency H3.3 G34R/V mutations in cortical pHGG. This unexpected finding provided the first clear evidence of distinct molecular subgroups of pHGG and indicated the importance of epigenetic dysregulation in this disease. Subsequent studies from our group and others continue to identify selective molecular signatures associated with pediatric glioma subgroups. Our current research addresses critical unanswered questions about disease pathogenesis of pHGG, including the role of cell type and developmental context in childhood gliomas, how histone mutations and epigenetic dysregulation contribute to tumorigenesis, and how plasticity and heterogeneity of tumor cells impacts tumor biology and therapeutic vulnerabilities.
Exploring the connections between brain tumors and CNS development
Why do specific mutations appear to confer a unique selective advantage in particular developmental contexts? We establish and leverage genetically engineered and patient-derived model systems that recapitulate developmental context to investigate the functional consequences of mutations and pathways critical to HGG. We are investigating in vivo comparisons of different cell populations and developmental time points to determine how mutations that are important in pHGG affect development, cell lineage and cell state and how this contributes to glioma growth, development and therapeutic vulnerabilities.
Molecular mechanisms and therapeutic targets in pediatric HGG
Genetically engineered models including patient-derived orthotopic xenografts and primary cultures provide critical insights related to tumor heterogeneity and therapeutic vulnerabilities. Introduction of pHGG mutations or disruptions of critical signal transduction pathways through gene editing, knockdown or chemical inhibitors in model systems are coupled with molecular and biochemical approaches to dissect mechanism and identify potential therapeutic targets. Integration of complex data sets from RNA-seq, single cell profiling, ChIP-seq, and additional platforms is central to our efforts to dissect molecular mechanisms.
We established a large collection of patient-derived xenograft models that we deploy for mechanistic studies and preclinical testing of potential therapeutic targets.

Selected publications
Contact us
Suzanne Baker, PhD
Member, Center of Excellence in Neuro-Oncology Sciences, Dept. of Developmental Neurobiology
Endowed Chair in Brain Tumor Research
Co-Leader, Neurobiology and Brain Tumor Program, Comprehensive Cancer Center
MS 323, Room M3412
St. Jude Children's Research Hospital
Memphis, TN, 38105-3678 USA GET DIRECTIONS