St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Gene therapy cures SCID
By using a unique type of gene therapy vector and treatment process, St. Jude announces a cure for SCID patients without a matched sibling donor.
Gene therapy developed at St. Jude is driving a landmark cure for patients with X-linked severe combined immunodeficiency (SCID-X1).
Sometimes called "bubble boy disease," severe combined immunodeficiency (SCID) is an inherited disorder that affect a person's genes. This genetic mutation affects white blood cells, mainly T cells, B cells and NK cells. These cells help the body fight off infections and protect against bacteria and other invaders. For infants who have SCID, these cells may be missing or may not work correctly. Infants born with SCID have problems fighting infections because the disease leaves them with little or no immune protection.
Previous treatments relied on bone marrow transplants from a matched sibling donor, but 80% of patients do not have a match. St. Jude researchers wish to provide a treatment option for patients without a bone marrow match. Patients with no matched donor have a lower rate of cure and may be at a higher risk of developing serious treatment-related side effects later in life.
Gene therapy offers hope of a cure
Scientists at St. Jude developed a novel gene therapy for children born with a rare immune disease
Featured research: A cure realized
Research led by St. Jude in collaboration with UCSF Benioff Children’s Hospital San Francisco has confirmed a cure. Building on the work of the late Brian Sorrentino, MD, of the St. Jude Department of Hematology, 10 infants diagnosed with SCID-X1 have received the experimental therapy. Results from the first eight patients have been published in the New England Journal of Medicine.
Our research is ongoing.
Featured clinical trial: LVXSCID-ND
Designed to restore the immune system in children diagnosed with SCID-X1, this clinical research study aims to correct an abnormality in the interleukin-2 receptor subunit gamma (IL2RG) gene in an affected child’s bone marrow cells. Eligible children have newly diagnosed SCID-X1, under 2 years of age and have had no prior treatment with allogeneic stem cell transplantation.
History of gene therapy for SCID
1993
Arthur Nienhuis, MD, St. Jude CEO, establishes experimental hematology program with a focus on developing gene therapy for blood disorders.

1998
In a first, St. Jude researchers led by Brian Sorrentino, MD, use gene therapy to cure severe combined immunodeficiency (SCID) in an animal model.
2000
French researchers report first X-link SCID (SCID-X1) patients cured by gene therapy.
2002
Leukemia surfaces as a treatment-related complication of SCID-X1 gene therapy. Gene therapy trials in the U.S. and elsewhere are halted.
2009
St. Jude researchers and colleagues develop a self-inactivating lentiviral vector based on the HIV virus to make SCID-X1 gene therapy safer and more effective. Investigators also streamline vector production.
2014
An international study with a different viral vector partially restores immune protection in infants treated for SCID-X1. Treatment-related leukemia is not reported.
2016
Investigators led by Harry Malech, MD, of the National Institute of Health, use the St. Jude SCID-X1 gene therapy vector to restore complete immune function in adolescents with SCID-X1 who were not cured by bone marrow transplantation.
2019
Investigators at St. Jude and UCSF Benioff Children's Hospital San Francisco use novel treatment that combines gene therapy and low-dose chemotherapy with busulfan to restore complete immune function in infants newly diagnosed with SCID-X1.

Featured stories
Gene therapy: A second chance
Samuel Evangelista was only 3 months old when he was diagnosed with SCID-X1. Once her doctor realized that treatment options were limited in their home country of Brazil, they contacted Ewelina Mamcarz, MD, of St. Jude Bone Marrow Transplantation and Cellular Therapy.
Mamcarz worked with the late Brian Sorrentino, MD, and his team in Experimental Hematology, who developed a lentiviral vector, which is a type of virus that inserts a copy of the healthy gene into the cells. This vector has helped patients like Samuel reconstitute their immune systems and live their lives without constant immunoglobulin infusions.

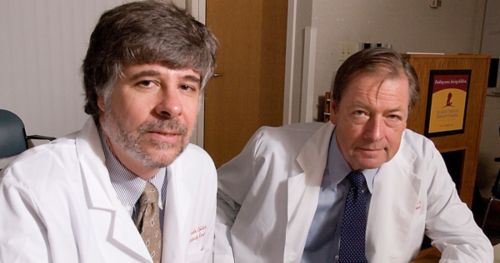
With Brian Sorrentino, it was about more than just the science
Arthur Nienhuis, MD, brought Brian Sorrentino, MD, to St. Jude in the 1990s to help start a new, leading-edge research department, Experimental Hematology. Sorrentino spent more than two decades searching for a way to use gene therapy to cure children with X-linked severe combined immunodeficiency (SCID-X1).
Three years after launching an innovative gene therapy clinical study, Sorrentino died of lung cancer, a late effect of high-dose therapy he received as a teenager for the treatment of Hodgkin lymphoma. But shortly before his death, Sorrentino reviewed final drafts of the paper confirming a complete cure of SCID-X1.
Nienhuis reflects on Sorrentino’s ability and skill as a scientist, but also his mastery of being able to bring people together to achieve something that truly makes a difference.

More information