St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
St. Jude Family of Websites
Explore our cutting edge research, world-class patient care, career opportunities and more.
St. Jude Children's Research Hospital Home

- Fundraising
Testing Evidence-based Strategies to Improve HPV Vaccination Coverage in Rural Primary Care Clinics
June 2023
By Natoshia M. Askelson, MPH, PhD and Shelley Walker
When it comes to HPV vaccination coverage, rural health clinics have not benefited from the extensive efforts to encourage strong provider recommendations for the HPV vaccine and clinic-based interventions that can support changes in clinic practices and policies. The reasons for this deficit are complex. For the most part, national and state organizations have focused efforts on health systems and practices with larger numbers of patients.
Early HPV vaccine promotion focused on pediatricians who typically do not practice in small, rural clinics. Rural clinics may not have large professional networks, so their clinicians are less likely to learn about effective methods for promoting the HPV vaccine. Rural health clinics are often not part of a larger health system and do not have access to the same resources as those in larger health systems. For example, rural health clinics could lack information technology support for electronic health records or staff dedicated to quality improvement.
Due to these challenges, more emphasis needs to be placed on reaching rural clinics and adapting existing effective interventions for these settings.
“We see a future where cervical cancers can be nearly eliminated in the U.S., sparing millions of women and families unnecessary pain, stress and financial burden. We believe that by working together over the long-term, we can move toward ending vaccine-preventable HPV cancers as a public health problem.”
—Shelley Walker


“HPV vaccination needs to be offered to all kids. Access to the vaccine should not be limited to just those clinics that are well resourced or have staff dedicated to implementing new initiatives and quality improvement. We need to tailor our clinic-based interventions to reach all clinics.”
—Natoshia Askelson, MPH, PhD
In collaboration with our partner, the American Cancer Society (ACS), we used state immunization registry data and the list of Vaccines for Children liaisons to identify rural clinics that were not in larger health systems and were in areas with low HPV vaccination rates.
We recruited 2 small health systems with 3 clinics each to participate with ACS in an intervention that included:
- Support for quality improvement
- Training and technical assistance
- Performance evaluation
The University of Iowa Cancer Prevention and Control Research Network Center conducted an evaluation to understand the implementation of the intervention. Preliminary findings after the first year of the intervention indicated some increase in initiation of the vaccine (see Figure 1).
Major barriers included:
- Insufficient numbers of staff to attend intervention meetings and implement the changes
- Challenges related to COVID-19
- Inability to efficiently use the electronic health record system
The intervention was extended for an additional year to allow the clinics more time to complete their projects. Final evaluation data are being collected. So far, data continue to point to the challenges of being a small, rural health clinic with limited resources. Rural clinics require significant support and time to successfully implement interventions to increase HPV vaccination.
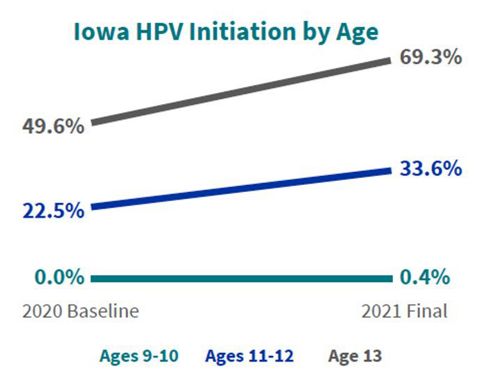
Figure 1. HPV initiation rates for 6 rural primary care clinics not associated with a larger health system.
Natoshia M. Askelson, MPH, PhD, is an Associate Professor, Community & Behavioral Health; Senior Research Fellow, Public Policy Center, and Interim Associate Director for Community Outreach & Engagement, Holden Comprehensive Cancer Center
Shelley Walker is associate director of State Partnerships at the American Cancer Society (ACS). The emphasis of her work is to impact the entire cancer care continuum through engagement with payors and government and state associations.
Through collaboration with partners, Walker aims to accomplish greater outcomes in cancer prevention through policy, strategy and technical assistance. The University of Iowa's Cancer Prevention and Control Research Network (UI CPCRN) has a focus on improving cancer outcomes in rural communities in Iowa. Through the ACS partnership, UI CPCRN has worked to increase HPV vaccination uptake through quality improvement efforts. This project focused on addressing the unique challenges faced by rural health systems such as understaffing, client insurance barriers, EHR challenges and provider accountability.
We invite guest contributors to share information on how they are working to improve HPV vaccination in rural areas. If you are interested in contributing or learning more about our efforts to improve HPV vaccination with rural communities, please email us at PreventHPV@stjude.org.